Dive Brief:
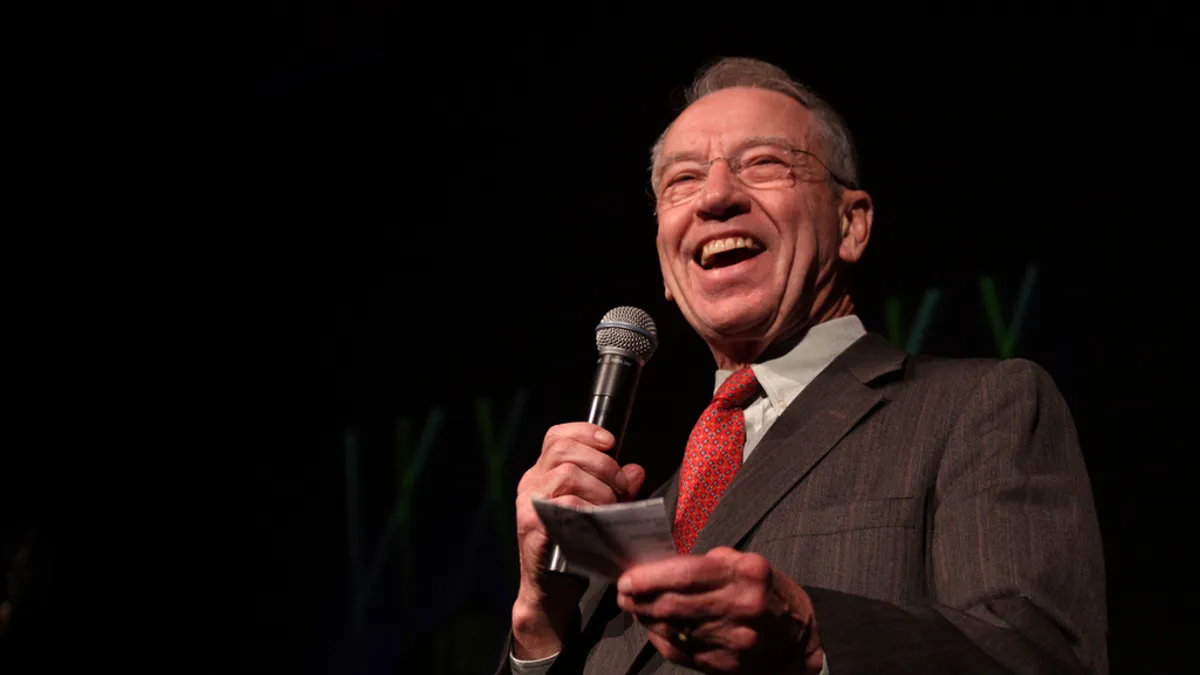
- Senate Finance Committee Chair Chuck Grassley detailed six questions to Trump administration officials after a government watchdog report found CMS may be inadvertently overpaying billions in Medicare payments for laboratory services.
- The Iowa Senator in a letter to HHS Secretary Alex Azar and CMS Administrator Seema Verma called out one estimate in the Government Accountability Office that a CMS policy on calculating baseline payment rates could result in "staggering" costs to taxpayers.
- A GAO official told MedTech Dive it stands by the report after the American Clinical Laboratory Association and AdvaMedDx called the underlying assumptions for GAO's analysis flawed.
Dive Insight:
In theory, the Protecting Access to Medicare Act was meant to cut costs by transitioning Medicare reimbursement to a system that reflects market rates, with rate reductions limited to 10% annually from 2018 through 2020.
But in its November report, GAO raised concern CMS' method to collect private market data from labs could result in inaccurate Medicare payment rates. In addition, it flagged the CMS decision to use maximum Medicare payment rates in 2017 as a baseline rather than actual payment rates as a concern.
"GAO estimated that Medicare expenditures from 2018 through 2020 may be $733 million more than if CMS had phased in payment-rate reductions based on the average payment rates in 2016," the report said.
Citing that report, Grassley also raised concern CMS could potentially cease paying a bundled rate for certain panel tests, instead of paying individual rates. GAO estimated that Medicare expenditures could increase $10.3 billion from 2018 to 2020 as a result.
But HHS claimed it was simply trying to comply with PAMA requirements to GAO. In a November letter, the department said it is considering adding new approaches such as adding codes to the Clinical Laboratory Fee Schedule and other actions to address the bundled payment issue. But it is unclear if those ideas appease Grassley.
"Given the significant expense associated with paying individual rather than bundled rates for panel tests, it is unclear why HHS did not undertake this analysis sooner," Grassley wrote.
ACLA contends PAMA implementation has instead resulted in millions of reimbursement cuts. The lobby appealed its lawsuit against HHS in December to the U.S. District Court of Appeals for the District of Columbia Circuit, which argues HHS overstepped its statutory authority implementing PAMA.
"Clinical laboratories are required to bill Medicare according to the American Medical Association CPT guidelines, which provide clear direction on how to report certain tests and disease panels. Rather than acknowledging these current standards, GAO concocts a hypothetical scenario that suggests labs are unbundling these tests and receiving higher reimbursement," Julie Khani, ACLA president, said in a statement in response to the GAO report.
And AdvaMedDx spokesperson Elyse Petroni told MedTech Dive the trade association is in the process of finalizing a formal letter to GAO outlining concerns with its report.
Despite industry's concerns, the government watchdog has confidence in the report's methodology.
"We stand by our report and its findings. I had not seen the [Grassley] letter and do not have any comments on it," James Cosgrove, GAO's healthcare director, told MedTech Dive in an email.