Dive Brief:
- The American Hospital Association in a new report estimates the financial fallout from the COVID-19 pandemic, and the numbers are sobering: It forecasts losses will top $200 billion — and that's just for the first four months of the outbreak from March estimated through June.
- AHA said the hemorrhaging can be connected to the cost of treating COVID-19 patients; losses from canceled surgeries and other services; the cost of buying additional personal protective equipment; and the cost of supporting frontline healthcare workers. The biggest slice of these losses comes from canceled surgeries, outpatient care and ER visits — estimated at $161 billion collectively.
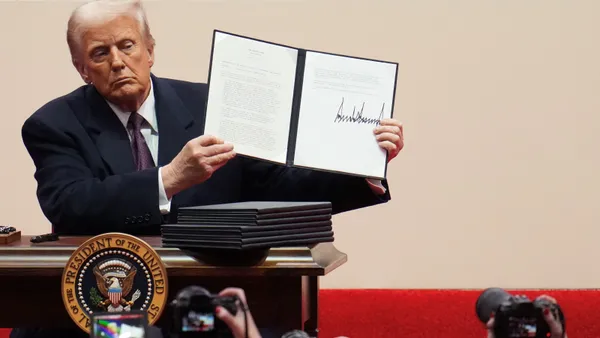
- The trade group is citing the figures in their ongoing bid for additional aid from Congress. Thus far, the industry has received about $175 billion in funding from the Coronavirus Aid, Relief, and Economic Security Act and other rescue bills. The survey suggests that many hospitals, which operate already operate on relatively thin margins, may not be able to survive without additional aid from the federal government.
Dive Insight:
The pandemic has been an enormous stressor on every aspect of healthcare delivery, but perhaps no sector has been hit as hard as hospitals. Not only have they lost tens of billions in revenue due to canceled elective procedures, but they have also had to spend more to treat coronavirus patients, the most seriously ill of whom can require weeks of treatment in intensive care units.
AHA has been pushing for additional aid beyond the initial $175 billion. With the Senate in session but the House out, it doesn't seem an additional package is imminent.
Now the group is putting a price tag on just the first four months of responding to COVID-19: $202.6 billion, or more than $50 billion per month.
The group's methodology relied on its hospital finance internal databases, while for treatment cost estimates it cited published data from the Kaiser Family Foundation and FAIR Health, and the Society for Healthcare Organization Procurement Professionals for the cost of PPE. It also noted that adjusted discharges, for both inpatients and outpatients, have dropped 13% from a year ago, a stark reversal from years of steady increases.
Major chains such as Tenet, HCA and Community Health Systems confirmed such plunges in their quarterly earnings reports, although they indicated that elective procedures should start up soon, spurred on in part by physician lobbies such as the American College of Cardiology.
The survey also observed that managing the current drug shortage, increased labor costs, buying new medical equipment such as respirators and costs related to reconfiguring hospital spaces to treat COVID-19 patients was also adding to losses, although AHA was unable to quantify specific sums yet.
However, the organization was unequivocal about what it will need to keep its members afloat over the long-term: more funding. It noted that the number of uninsured could rise to as high as 40 million — approaching pre-Affordable Care Act numbers — which could also lead to more charity care and write-offs.