Stryker’s procedure volumes and capital equipment demand remained strong in the third quarter, fueling nearly 10% sales growth amid the company’s “sprint back to 2019,” CFO Glenn Boehnlein said Thursday.
Issues that plagued the sector for the first years of the COVID-19 pandemic, like hospital staffing pressure and supply chain problems, are still challenges, but are getting closer to pre-pandemic norms. Stryker also reported strong procedural demand, with a backlog expected to boost orthopedic surgeries through 2024.
While executives were positive about 2024 procedure trends and product launches, they would not answer questions on specific projections, instead telling investors on a Thursday after-market earnings call to wait until January.
CEO Kevin Lobo said that the normal seasonal cycle of procedure demand is returning after the “turbulence” of the past few years. Strong seasonal demand has already begun in the fourth quarter, similar to 2017-2019, he noted.
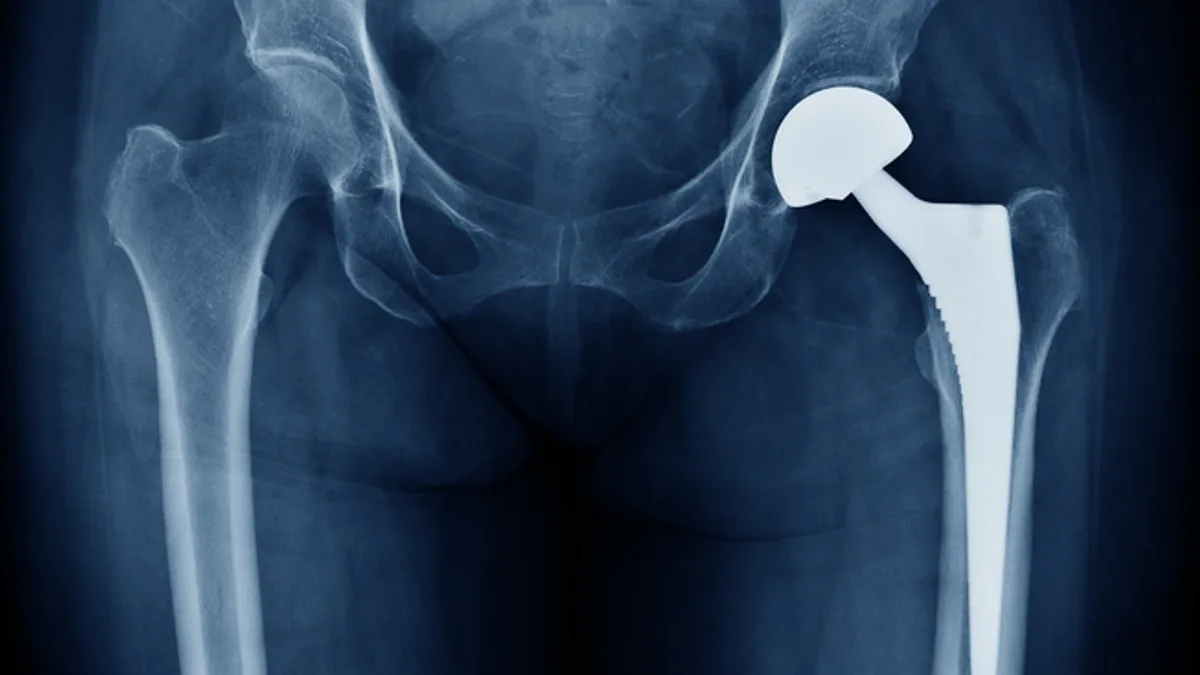
“We're already seeing that with the month of October. So, I think we're doing fine. Our business did not surprise us in terms of the results that we had. Obviously, we had giant comps from [Q3] last year,” Lobo said on the earnings call. “I feel very good about our position in both hips and knees and expect to have a good fourth quarter.”
Stryker’s sales in the third quarter grew approximately 10% to $4.91 billion, with growth in both its orthopedics & spine and medical-surgical & neurotechnology segments. Executives mentioned several times on the call that along with solid procedure volumes, there is a strong backlog for capital equipment.
The company beat analysts’ expectations in the quarter by $45 million, according to a J.P. Morgan note. The analysts wrote that new product sales helped Stryker’s instruments and endoscopy businesses outperform Wall Street’s estimates, offsetting misses of $46 million and $22 million in the company’s medical and large joints businesses, respectively.
A more stable — and dependable — supply chain is also benefiting Stryker. Boehnlein said good visibility on the supply chain and raw materials purchases has helped the company’s gross margin.
“That means we can get back to things like ocean freight and not air freighting all the time. We can have regular manufacturing scheduling and cadence, which means that we don't have people cycling in and out, which is really inefficient,” Boehnlein said.
Stryker will provide more insights into current trends and where businesses stand next Wednesday during an investor day event.
One topic that will be addressed next week is the ongoing concern across the industry about how the obesity drug craze will impact device companies. Lobo did not go into detail on the topic, saying that a surgeon would discuss weight-loss drugs next week, but he did not hesitate to write off the medications’ potential impact on Stryker’s businesses.
“The studies saying that there's going to be a reduction, I think, are nonsense,” Lobo said. The CEO added that he has recently spoken with “multiple surgeons at massively credible teaching hospitals — world-renowned teaching hospitals — who have pored through the research and feel that there is no need for us to worry whatsoever about any slowdown in our knee procedures.”
Lauding ASCs
Stryker has recently used ambulatory surgery centers, especially over the past three years as companies searched for alternative sites for procedures amid the fall in surgeries conducted at hospitals. The trend appeared during a growth in robotic surgery among orthopedic companies.
Now, ASCs may be a key growth drive for ortho robots, like Stryker’s Mako system. Lisa Kloes, general manager of Stryker’s knee business, said in a recent interview with MedTech Dive that the company has more than 300 Mako systems in ASCs.
Lobo told investors Thursday that about 12% of Stryker’s hip and knee procedures are done in ASCs, and that number is “growing dramatically,” opening the door for “tremendous upside” in growth for Makos in the centers.
The CEO explained that there is strong demand in the U.S. but also in Europe, as countries like Switzerland, Germany and the U.K. are “starting to figure out that this model is actually a good model for the delivery of health care.”