Dive Brief:
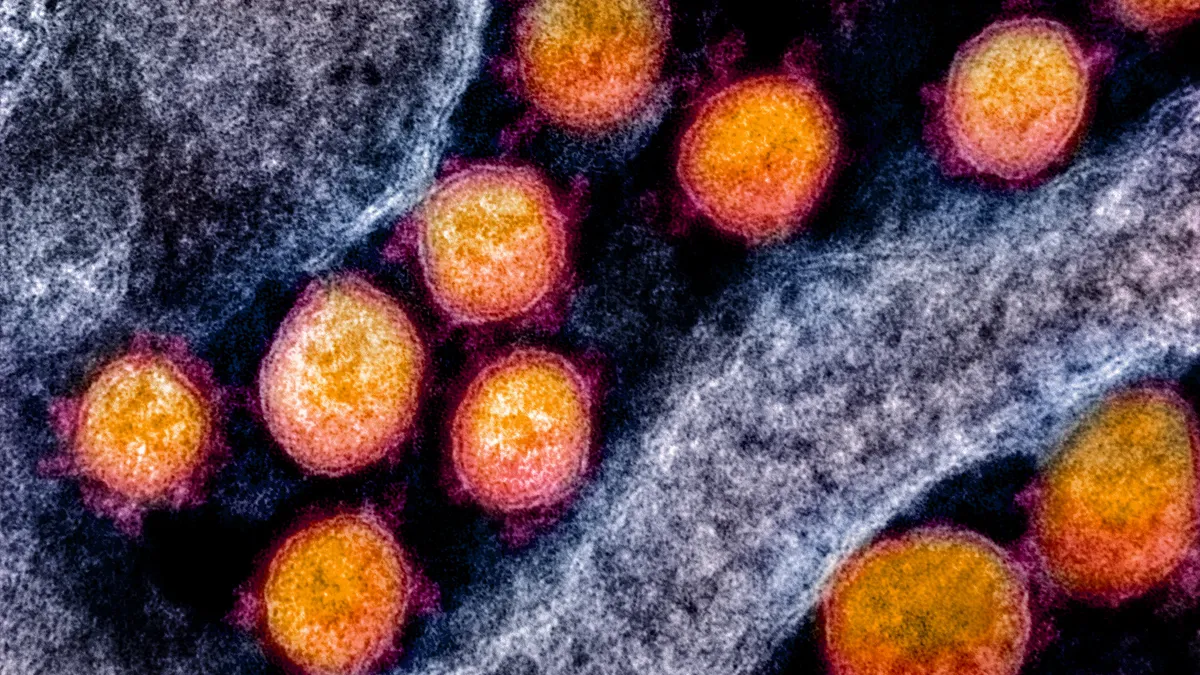
- The Association for Molecular Pathology and the Infectious Diseases Society of America are cautioning healthcare providers against using certain data generated by some COVID-19 PCR tests to make patient care decisions.
- Some tests generate data known as cycle threshold (Ct) values that have the potential to help determine a patient's prognosis and risk of transmission. But the wide variety of testing procedures in use and lack of a universal threshold are barriers that could result in misinterpretation of results and mismanagement of patients, the groups warned in a blog post.
- Separately, the American Clinical Laboratory Association issued a white paper on Thursday recommending that molecular tests that detect SARS-CoV-2 nucleic acid, such as PCR tests, should be prioritized for diagnosing COVID-19 in symptomatic patients.
Dive Insight:
Demand for COVID-19 testing wavered in the first quarter as vaccination efforts began to ramp up, according to companies making the tests and laboratories that process them. Still, executives expect testing to continue to play an important role in public health efforts alongside vaccine rollouts for the foreseeable future. Schools, workplaces and other venues welcoming people back will rely on screening procedures to prevent virus resurgence.
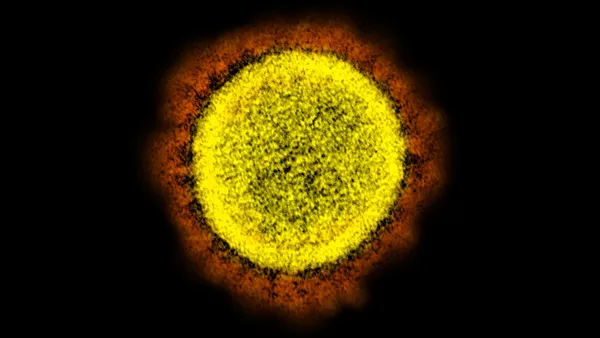
The ACLA, whose members include LabCorp and Quest Diagnostics and sell a range of tests, advised in its white paper that screening programs using tests on a frequent basis that provide quick results can help contain community spread of the virus. Nucleic acid amplification tests, which include PCR assays, should be the "tests of choice" for symptomatic patients because they provide a definitive diagnosis. However, about 33% to 45% of people infected with SARS-CoV-2 are asymptomatic, ACLA said.
Antigen tests, which have lower analytic sensitivity, can be used if nucleic tests are not available, ACLA said. But the group noted that "there are many businesses, airlines and even countries that will only accept PCR tests based upon a belief that only PCR test results can be used to diagnose COVID-19. This misconception places an unnecessary burden on labs and resources."
ACLA recommended that federal agencies such as the CDC and FDA provide more education on the appropriate use of NAAT tests. The group said data show that the reliability of antigen testing increases the more frequently a person is tested. Those who test positive with an antigen test should have the results confirmed with a NAAT.
Meanwhile, growing interest in using Ct values to measure the amount of SARS-CoV-2 in clinical specimens prompted AMP and IDSA in March to issue a joint statement on the use of Ct values in clinical decisions. In a follow-up blog post, the groups recommended that healthcare providers avoid routine use of Ct values to make clinical decisions because currently available data is limited.
Expanded development and standardization of test methods and more rigorous clinical data is needed, the groups said. For now, use of all qualitative tests currently on the market, including those that do not generate a Ct value, avoids potential bottlenecks that could result from demand for tests reporting Ct value.
According to the CDC, the correlation between Ct values and the amount of virus in an original specimen is imperfect, for both qualitative and quantitative PCR assays. "It is therefore problematic to infer any relationship between an individual patient’s Ct value and their viral load," the agency said. Ct values also can be affected if a specimen is not collected or stored properly or was collected early during the infection, the CDC said.