Dive Brief:
- A new CMS code would make it easier for digital therapeutics companies, like Pear Therapeutics, to get reimbursed for their software-based treatments. The CMS published a new Level II Healthcare Common Procedure Coding System (HCPCS) code for "prescription digital behavioral therapy," which could make it easier for commercial and Medicaid plans to cover these therapies. It will go into effect in April.
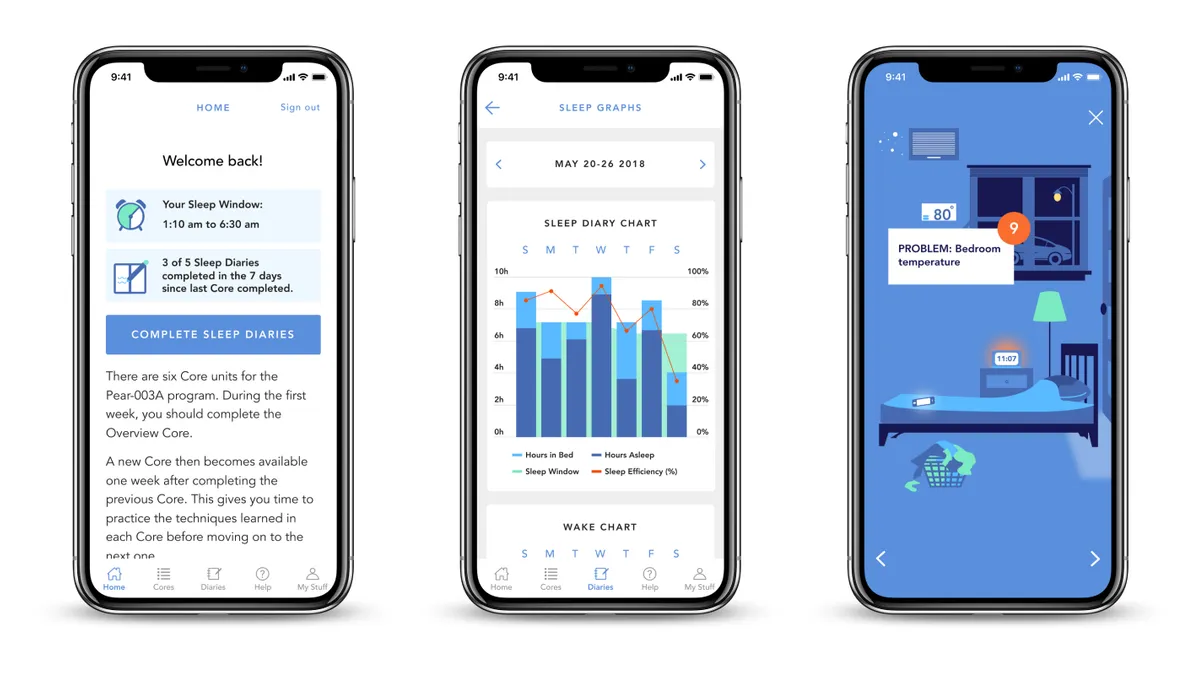
- For Pear, this would apply to its app-based treatments for addiction treatment and insomnia, which are FDA-cleared. Although more digital therapeutics are getting FDA indications, companies are still figuring out what payment models work best.
- Pear, which went public in December through a SPAC merger, hasn't yet reported its 2021 earnings. In January, the company shared it had met its target for the year to have 14,000 prescriptions for its products. The company initially set guidance for $4 million in revenue in 2021 and hopes to increase that number to $22 million in 2022.
Dive Insight:
For Pear to meet its revenue targets for 2022 — nearly five times what it brought in last year — the company will need to make it easy for physicians to prescribe its digital therapeutics and get reimbursed. The new CMS code is seen as an important step in that direction.
At Citi's Healthcare Conference on Thursday, Pear CEO Corey McCann said the HCPCS codes would serve as another option for payers to cover its digital therapeutics as a medical device. McCann also talked about plans to put forth legislation that would create a specific benefit type for digital therapeutics through the CMS.
"I believe that today's HCPCS code is a nice example of how CMS views PDTs [prescription digital therapeutics] as a discrete product type, and we may not even need the legislation ultimately, but it's really a belt and suspenders effort," McCann said.
McCann also claimed the company brought on two of the top five pharmacy benefit managers — Optum and Prime Therapeutics — although it is not listed on Optum's standard formulary. The partnership merely lets companies opt-in to make Pear's apps available to their employees. The CEO also said Pear has partnerships with some state Medicaid plans, including in Massachusetts, Oklahoma and Michigan.
In a Thursday note, BTIG analysts also pointed to a decision by the American Medical Association last year to clarify its CPT code for remote monitoring to include cognitive behavioral therapy, which would allow clinicians to be reimbursed for time spent checking patients' progress through dashboards. It's expected to go into effect in 2023.
"We believe this HCPCS announcement and other recent wins with state payors demonstrate that PEAR's efforts are leading to the gradual accommodation of [prescription digital therapeutics] within the framework of healthcare prescribing, billing, and reimbursement," the analysts wrote.
Boston-based Pear currently has three FDA-cleared digital therapeutics for substance use disorder, opioid use disorder and insomnia. While they're intended to be prescribed like a medication, patients download the app and work through a series of modules. Pear also is working on a platform to host multiple digital therapeutics, making it easier to integrate them into clinicians' electronic health record systems.
When asked why Pear chose to go down this route of seeking reimbursement from insurers, which has involved carving out new payment models, McCann said it was not a choice for the company.
Pointing to the number of digital health companies that are seeking out employers as customers, the CEO said, "What you have today is a whole host of unregulated products that target relatively healthy normals and that do so for the service of self-insured employer groups ... It's a relatively small section of healthcare and has become a relatively congested portion of the healthcare market."
McCann added that while there's nothing wrong with that model, Pear would need an FDA label because the company sought to provide treatment for more high-acuity conditions. Many of these patients also are covered by traditional commercial insurance plans or state Medicaid plans.
"And so really, if you work backwards from the answer, our goal was to make software mainstream medical treatment," McCann said. "We believe that if you want to make software mainstream medical treatment, you go down the path that we've gone down."
Looking to 2022, McCann said that coverage density will be key, meaning that the company plans to build out areas where the majority of patients who receive a prescription contribute to its revenue. For example, in Massachusetts, every Medicaid patient in the state has access to its reSET and reSET-O therapeutics. Pear is looking to make similar agreements with other states and commercial payers.
Correction: This story has been updated to clarify the nature of Pear's relationship with Optum, which is narrower than being listed on its standard formulary.