Dive Brief:
-
Medicare unnecessarily paid $34 million to suppliers of prosthetics, braces and other medical equipment from 2015 to 2017, a government watchdog report found.
-
The improper billing, which also cost patients $8.7 million, stemmed from the inadequacy of the CMS' systems that should have stopped or detected the overpayments, according to the Office of Inspector General.
-
OIG wants CMS to oversee the recovery of the $34 million and refunding of patients, while also working to fix systems it thinks have cost the government $223.1 million since 2008.
Dive Insight:
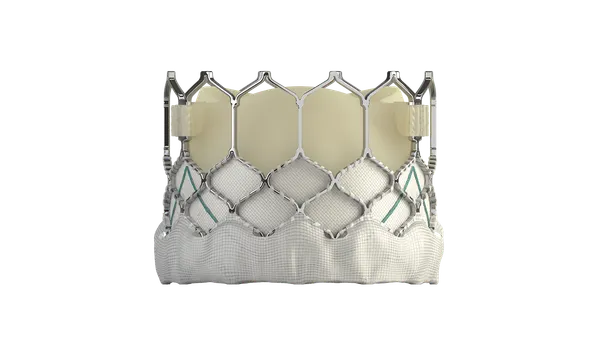
OIG has previously trained its sights on improper payments for services provided to patients cared for at acute-care hospitals and other types of inpatient facilities. However, these earlier investigations paid little attention to durable medical equipment, prosthetics, orthotics and supplies (DMEPOS), a catch all term for devices including wheelchairs, artificial limbs, braces and other products.
Generally, Medicare should not pay suppliers for these items. Instead, the items should be covered by the Part A payments Medicare makes to inpatient facilities. DMEPOS devices are not separately billable.
To assess whether the system is working as intended, OIG reviewed $34 million in Part B payments Medicare made to suppliers for 120,000 DMEPOS claims in 2015, 2016 and 2017. OIG concluded that none of the claims it assessed should have been paid by Medicare, meaning CMS unnecessarily gave $34 million to suppliers over a three-year period.
The overpayments should have been detected by the system CMS uses to verify, validate and authorize claims. However, OIG found the system was not designed to include certain types of DMEPOS items, including prosthetics and orthotics.
That shortcoming has proven to be costly. Having reviewed claims made over the three-year window, OIG looked at DMEPOS items billed during inpatient stays going back to 2008. The review found the annual level of overpayment fell from around $30 million a decade ago to just over $10 million in 2017. Medicare DMEPOS overpayments for the past 10 years total $223.1 million, which could have cost beneficiaries $56.3 million in deductibles and coinsurance, according to OIG.
OIG has asked CMS to recover the $34 million and recommend that suppliers refund patients up to $8.7 million in incorrectly collected deductibles and coinsurance amounts. OIG wants CMS to take “all necessary actions,” including seeking legislative authority, to get suppliers to pay back patients. However, OIG made no mention of trying to recoup the rest of the $223.1 million incorrectly paid by Medicare since 2008.
The other OIG recommendations are intended to stop Medicare overpaying in the future. With that in mind, OIG wants CMS to ensure prosthetics and other DMEPOS are included in its overpayment detection system.
CMS agreed with all bar one of the recommendations. The exception was the suggestion that CMS seek legislative authority to get suppliers to refund patients. In response to the recommendation, CMS said it will consider whether to put the proposal forward for inclusion in the next budget.