Recent approvals for Abbott Laboratories and Medtronic to use their spinal cord stimulation devices to treat painful diabetic neuropathy are setting up competition for the millions of patients who, until recently, had few treatment options. But Nevro, the first company to receive approval from the Food and Drug Administration for the indication, expects to maintain a lead in this market based on its clinical trial results.
Redwood City, Calif.-based Nevro, whose spinal cord stimulation implants also treat back pain, had revenue of $406.4 million in 2022, and expects $445 million to $455 million in 2023. The company expects its diabetic neuropathy treatment will be a source of growth, along with the launch of its newest device, HFX iQ, which can tailor patients’ treatment based on their input.
Nevro is also searching for a new CEO, as its current chief executive, Keith Grossman, plans to retire.
Nevro’s chief medical officer, Dr. David Caraway, talked about the company’s growth strategy, competition with other spinal cord stimulation devices, and future plans for new products.
This interview has been edited for length and clarity.
MEDTECH DIVE: How does your spinal cord stimulation treatment work?
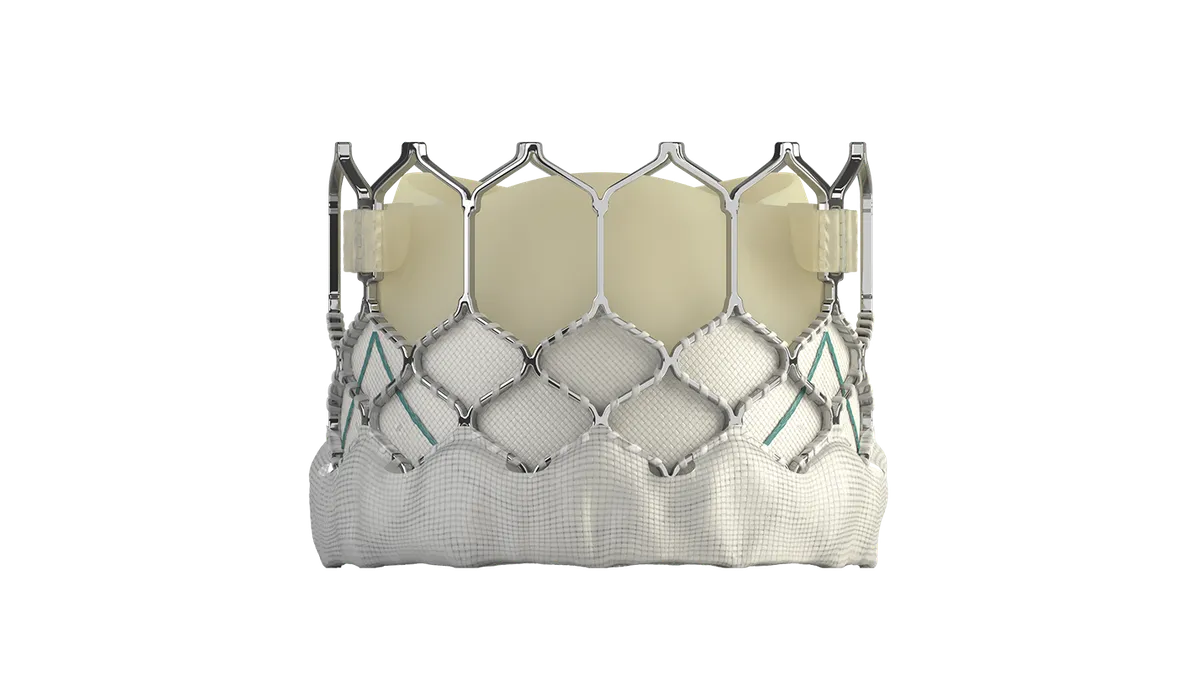
CARAWAY: There is conventional spinal cord stimulation that's been around for 40-plus years. I've put in hundreds of these devices back when I was practicing. And the way that works is you have these little electrodes that are on thin flexible wires, you put them in the epidural space, and you use small pulses of electricity to stimulate the sensory pathways in the spinal cord, [in] the dorsal column.
You stimulate those at a lower frequency, and what the patient perceives usually is a tingling sensation or a vibration — sometimes it can feel uncomfortable. What you try to do then is move those contacts around and program [it] in such a way that that tingling sensation, what we call paresthesia, is overlapping the area of pain. And the hope is that the tingling will mask the pain. That's the way stimulation has always been.
Well, when Nevro came out with paresthesia-free therapy, it's very different. [With] our therapy, patients don't feel anything and we don't activate these dorsal columns; we don't cause paresthesias. At the frequency we operate at, which is 10,000 Hertz, the patient doesn't feel anything, but at the spinal cord level it does inhibit those firing pain-circuit neurons and quiets them down.
How long do patients use it? Is it intermittent, or all day?
With traditional conventional spinal cord stimulation, the usual condition was you leave it on all the time, because when you turn the paresthesias off, there's the risk that your pain comes back.
Many of our patients, because they don't have any discomfort with it, can use it while they're driving, while they're sleeping. It doesn't interfere with any of those activities. So the majority of our patients just leave it running 24/7 and have very good results. Also, what we'll do with many patients is turn it off and on during the day because the effect of HFX therapy does last much longer than just the time that it's on.
You won FDA approval in 2021 to use your device to treat painful diabetic neuropathy. Since then, Medtronic and Abbott have added that indication. How are you thinking about the competition?
Medtronic got an approval based on these older studies. They used those and combined them with some safety findings and hard data to achieve an indication approval. Abbott did the same thing, sort of the “book report” approach to FDA approval. Those studies have been out there for 10 years and never moved the needle, either with the FDA or with payers, which is important, right? The therapy's no good if you're not going to get it paid for.
On the other hand, the strength of our evidence is what moved the needle. We got the FDA indication, and had payers begin to understand this. So we're proud of that.
What are your expectations for adoption of your painful diabetic neuropathy treatment?
There's something like 18 or 19 million people with diabetes who go on to develop diabetic neuropathy. And of those folks, of the diabetic neuropathy patients, about half of them have painful diabetic neuropathy. So it's a large cohort, and 45% of those [people] fail medications or can't tolerate them. So it's a sizable problem that we are interested in solving. Historically, conventional spinal cord stimulation has been used, but with mixed results. Here you are treating patients who have painful paresthesias with more paresthesias, and they just don't like it. And that's sort of what the studies have shown out.
We have high expectations, and I think for good reasons. In our randomized controlled trial, we picked patients who look like the standard [painful] diabetic neuropathy patient. We compared our treatment to medical management by experts. And we had really tremendous success.
[We’re] the only ones that had the foresight to make the investment in putting together a large-scale database from which we can do big data dives and develop algorithms. That's what this was all about.

Dr. David Caraway
Chief Medical Officer, Nevro
We expect that patients who receive this therapy, if they're appropriate candidates, a very high percentage [should] do very well with at least a 50% pain reduction, and on average, in our study, [they showed] almost 80% pain reduction. So that's a big improvement for these folks. The challenge for us, and for the clinicians who treat these patients, is awareness. This is new; they're not aware of this.
Many of these patients are managed through primary care and endocrinology, and they work carefully on their metabolic issues. But once they've given them pregabalin, and gabapentin and duloxetine — these two or three medicines that are approved for treatment — they've got nothing left to offer. As I mentioned, only about half of the patients respond to that. And many of those patients who respond discontinue because of side effects.
So they have nowhere to go. And that's what we wanted to do is make sure that those patients who suffer so horribly, they're walking the floors at night, they're rubbing their feet, they can't even keep their bed covers on, so they're miserable, and they feel like their feet are burning — we have an answer for those patients.
How is insurance coverage?
There are seven Medicare [Administrative Contractors]. Five approved the therapy [for] PDN. And there are two that are pending. So I think that we'll have across-the-board Medicare coverage in the very near future. And many, if not most, of the major commercial insurers are also covering this with our therapy.

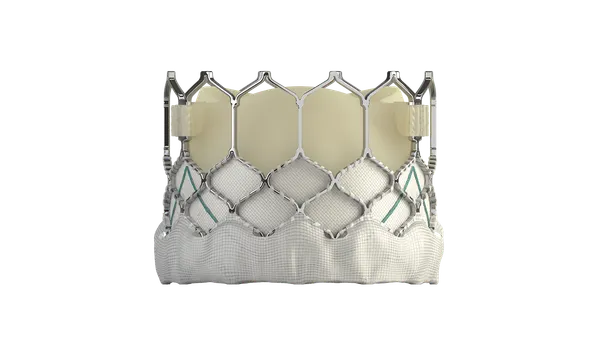
You recently started a full commercial launch of your newest device, HFX iQ, in the U.S. What makes it different from your other spinal cord stimulation system?
What we have now is really the first big-data-backed, AI-powered system that actually gets smarter over time by learning from the patient. The patient gives inputs, and we're able to start the patient off with the program that is most likely to help them. We can in real time, from the patient's responses, deliver personalized care right on the patient's application. So that's a first.
We've collected millions of data points, 80,000-plus patients in this first algorithm set, now over 100,000, to put together the algorithms that show patients of that particular sort of demographic and pain distribution, what [device settings] would start them off the best. And then we work through our algorithms so that as the patient puts in inputs [such as] “How are you doing today? What's your pain score? What are your medications like? What are the quality of life measures?” Every day we query them, and they put information [in], and then the system actually offers up recommended program changes, and the patient can then accept them. Then [the system] continues in this way learning and getting smarter over time. We're really excited about that.
What’s an example of how that would work?
Let's say the patient lives a couple hours away from the doctor's office. Formerly, without the iQ device, if your pain wasn't in good control, you'd have to call somebody [to] make an adjustment with them, get some guidance, get reprogrammed perhaps, to a program that works better for you. And maybe your pain has changed yet again by the time you get home from that reprogram visit. Pain is very dynamic. It can be hindering one day and fine the next. And it can change based on activity levels, on medication levels, so the iQ takes this all into consideration and then works with the patient as it learns.
What do you expect will drive Nevro’s growth in the future?
The PDN launch a year and a half ago, [in the] fall of ‘21, has been a big driver for us, and we anticipate that it’s just beginning.
Our core business has always been back and leg pain. We have proven superiority over conventional spinal cord stimulation for treating back and leg pain. And we continue to leverage that and to gain market share in that regard as well.
We recently brought another indication to market. We're the only ones that have an indication for what we call non-surgical refractory back pain. These are patients who are not candidates for back surgery; they've failed all the usual treatments like injections or interventional pain treatments and medications. So they're left in a bind as well.
We did a large scale randomized control on that group of patients and showed similar outcomes with that group, as you would see in so-called “failed” back surgery patients. So that's a whole other group of patients that we're working with insurance companies and payers to make sure we get [them] answers and coverage.
We're continuing to look at new indications as well. And then technology: I told you that iQ has been an enormous amount of work and technology to deliver, all predicated on being the only ones that had the foresight to make the investment in putting together a large-scale database from which we can do big data dives and develop algorithms. That's what this was all about.