It takes more than five years for breakthrough medical technologies to gain even partial Medicare coverage after approval from the Food and Drug Administration, research from the Stanford Byers Center for Biodesign at Stanford University has found. That’s keeping a whole segment of the U.S. population from benefiting, according to Dr. Josh Makower, director and co-founder of the Byers Center for Biodesign and a professor of medicine and bioengineering at Stanford.
Makower has been one of the leading voices urging the Centers for Medicare and Medicaid Services to find a way to get patients access to breakthrough devices.
As the founder and executive chairman of ExploraMed, a medical device incubator, Makower calls himself a serial innovator, having created nine companies since 1995, most of them in medical technology.
Makower, who recently testified at a Congressional hearing on medical innovation and getting patient access to the latest technologies, shared his thoughts on how to speed the approval of breakthrough devices and get the latest medical technology to the patients who need it.
This interview has been edited for length and clarity.
MEDTECH DIVE: Medical technology has been developing at what seems like breakneck speed these days, but a lot of devices and technologies that get fast-track FDA approval, what’s called breakthrough designation, take ages to get to the patients who need them most. Why is that?
MAKOWER: The primary issue that innovators are facing is payment/reimbursement. Unfortunately, Medicare is right in the center of setting the pace for coverage across the insurance ecosystem. Private insurers play a very substantial role, but Medicare has the opportunity to rethink processes that would help advance innovation to help reduce costs, and improve patient outcomes and patient access. This issue is what brought us to focus on this here at Stanford Biodesign’s policy program.
You were fairly instrumental in getting the FDA to fast track the approval of innovative medical technology. How did that happen?
When there’s something in the ecosystem that threatens the advancement of new therapies, it gets my attention. Back in 2008, the FDA process became dramatically more difficult to navigate for innovators as goal posts shifted and transparency and predictability suffered. At that time, we wrote a report on the financial and clinical impact of these changes, and the impact it was having on the medical innovation ecosystem. It took about two years of effort, ultimately resulting in passage in 2012 of the Food and Drug Administration Innovation Safety Act. That act prompted dramatic changes at FDA that are really evidenced now, and FDA is no longer one of the major inhibitors of the advancement of innovation.
What’s the current status of efforts by CMS to develop an expedited reimbursement pathway for emerging medical technologies?
This idea of an accelerated program for truly breakthrough therapies was first conceived during the Obama administration around the same time and has languished over several administrations. At the end of the Trump administration, Trump pushed through to CMS this policy called MCIT, Medicare Coverage of Innovative Technologies, and CMS essentially set it aside shortly after it was supposed to come into [effect].
The reasons for setting it aside were legitimate. There were many aspects of MCIT that were not thoughtfully considered, such as not requiring manufacturers to collect evidence during the temporary coverage period. MCIT, in short, would allow any breakthrough technology, as designated by the FDA, to receive at least four years of Medicare coverage very shortly after it receives clearance or approval. At the end of four years there would be a determination as to whether the technology would be granted permanent coverage. Such a program would be a huge stimulus for innovation and would allow Medicare beneficiaries immediate access to important breakthrough therapies deemed safe and effective by the FDA.
Unfortunately, in the original MCIT proposal, there was no discussion of the process around which this would actually be implemented. And no discussion of what additional resources might be necessary to make it successfully implemented. And as I mentioned, very little consideration for the fact that there needs to be probably a requirement to collect more evidence during this period to make sure that CMS has all the information it needs to render a permanent coverage decision. Many people supported MCIT and wished it could have proceeded, even if modified.
Since that time, CMS has said that they’re working on a proposal to address that need, which they have called TCET, Transitional Coverage of Emerging Technologies. At this moment, we have no idea what TCET is. I imagine it must be somewhere navigating the approval process for release, but we have not seen it yet. So we don’t really know whether this solves the problem and addresses the needs. At this moment, we’re hopeful that this proposal will solve some of the needs and get breakthrough technologies into patients’ hands earlier that have been approved as safe and effective by the FDA. But we don’t know.
How long does it currently take for medical device innovations to gain CMS reimbursement?
The data that I shared in my testimony show that the actual median delay for breakthrough-type technologies between approval is 5.7 years. This is a very long time for Medicare beneficiaries to wait.
This delay has a huge impact on the innovation ecosystem. During that 5.7 years or more, these businesses need to stay in business somehow. It’s not clear how they do that, to be able to deliver their therapy to the patients that they were created to serve, when they cannot derive any income. Until they have coverage, they cannot sell their products, because they cannot be reimbursed for those products or services. So it is a particularly troublesome thing, especially when considering that these are breakthrough, novel, new technologies that are meant to address a need that has not been really solved well before. Our work has been focused on trying to bring attention to this issue. And I was honored to be asked to testify at the House Ways and Means health subcommittee on this topic, because it should get our attention. It impacts everyone, regardless of their political leanings. This is something that does have bipartisan support.
What should Congress do to help improve reimbursement for new technologies?
Legislation could help provide resources, if necessary, to better support this program. Quite honestly, it took FDASIA, the Food and Drug Administration Safety and Innovation Act, to make it clear what Congress wanted the FDA to do with respect to the issues FDA was having at that time, and it sent a very strong message. I’m very pleased to say that, for the most part, FDA has performed to that legislation’s direction very well. At this moment with respect to the needs addressed by MCIT, this is an opportunity for Congress to speak, and send the agency a clear message about what it would like to do on. Even if it only results in leaders at the agency making new choices, that’s still a good outcome. I’m sure that more resources would be helpful and are probably needed to pull this off successfully at scale. From my perspective, as an innovator, as a physician, as a professor who trains people in this field, my students and fellows are making major life and career choices on how they’re going to pursue the advancement of healthcare. If we want them to go into the field of medical innovation, this needs to be fixed. It’s not working well now, and there’s just too much delay and too much waste. We really should find a way to make this work for patients and really for the future of innovation.
How has current policy affected patients and device makers?
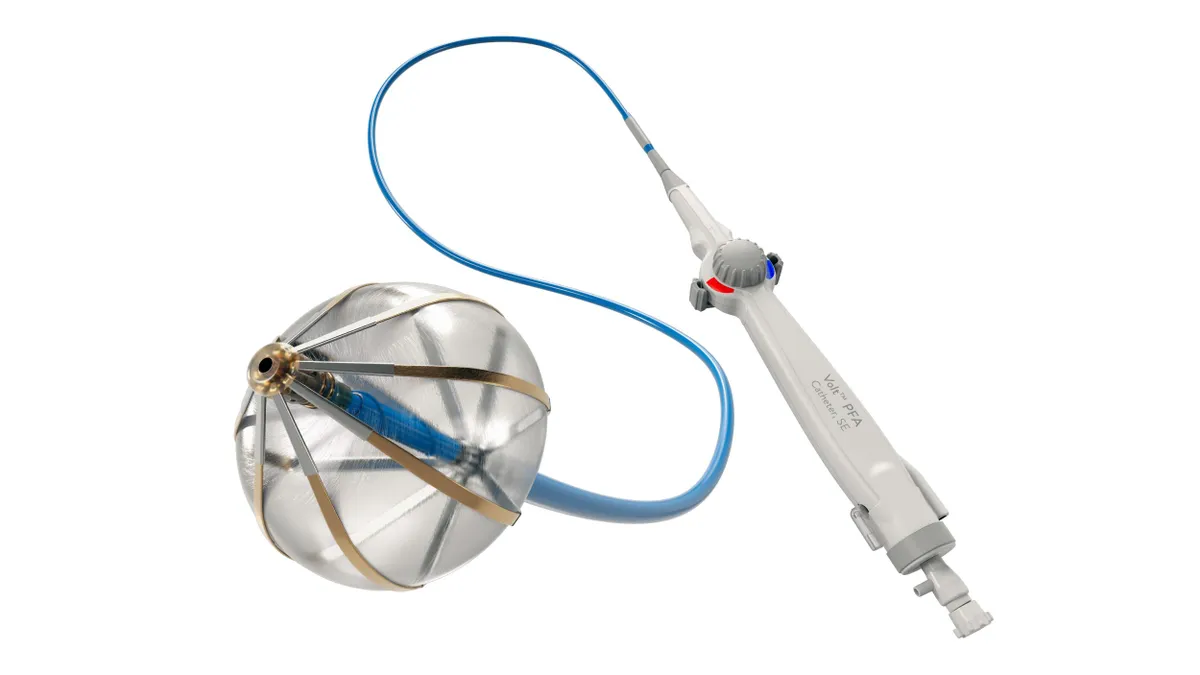
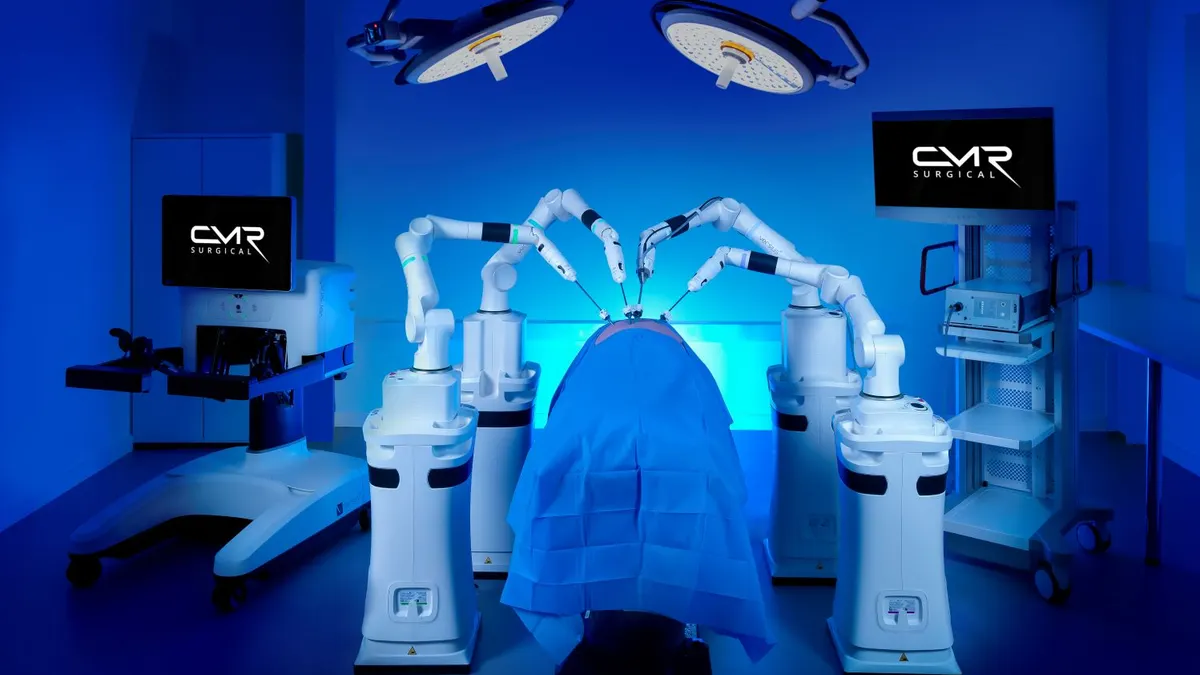
General categories of devices that took many years, at least four or five years, to get to some level of a minimum amount of coverage, are devices like continuous glucose monitoring, technologies for sleep apnea, or technologies to treat major ear, nose and throat diseases, or benign prostatic hypertrophy, one of the conditions that affects a majority of men over the age of 50, technologies for treating heart failure, or diagnostic technologies for cancer. Those are some of the things that have fallen into this group. The FDA has approved these devices and deemed them to be safe and effective.
Why wouldn't breakthrough devices solving important unmet clinical needs that are proven safe and effective by the FDA be covered under Medicare? CMS has a different standard that they call “reasonable and necessary.’” But that is not a very clear standard like “safe and effective” is. It would be great if one of the outcomes of this work is a much clearer framework for what is required to be deemed reasonable and necessary. At the moment, it’s a little bit of an opaque process. Fixing the reimbursement issue in this way would be helpful to advance medical therapy, because innovators have to make a plan, they have to raise money to create the opportunity, and if they’re wrong about how long things take, they could run out of money and patients would never get any of the benefit of these new innovations.
What might an expedited pathway for Medicare coverage look like?
We would love to see a modified MCIT proposal, one that provides for relatively immediate Medicare coverage for a clear and decent amount of time – four years is a nice amount of time – during which time there would be a requirement to collect certain evidence with an outcome clearly specified and negotiated with CMS about what additional data would need to be collected. [That way] CMS can make a reasonable permanent coverage decision. That’s what we’d love to see happen. It would provide a clear framework for innovators to work towards, and it would help maintain and sustain this fragile medical innovation ecosystem to advance new medical therapies for patients in need.
Updates to add additional information including the role of CMS in the setting of private insurance reimbursement rates.