Dive Brief:
- Hospitals, doctors and medical device manufacturers may soon be able to coordinate care more easily if a set of proposed rules aimed at easing compliance barriers to encourage value-based care released Wednesday morning are finalized.
- The long-awaited proposals from the Trump Administration seek to alter physician self-referral and anti-kickback laws to account for the healthcare system's shift from fee-for-service to value-based arrangements. Backers of the revamp say current regulations discourage providers from entering into partnerships aimed at improving quality outcomes due to fear of harsh criminal penalties.
- A number of new safe harbors are proposed to encourage value-based care, allow patient engagement through furnishing of certain tools and supports and permit certain remuneration when provided in connection with some CMS-sponsored models to cut down on the need for fraud and abuse waivers. They also provide guidance aimed at clarifying when compensation provided to a doctor by another provider must be paid for at fair market value.
Dive Insight:
Industry has been lobbying for changes they argue will improve care for patients and open new business opportunities. The American Hospital Association, American Medical Association and AdvaMed each submitted feedback when the administration requested ideas on how to alter the Anti-Kickback Statute and Stark Law in 2018.
The effort to reform the set of laws largely fell under the stewardship of HHS Deputy Secretary Eric Hargan, who has argued over the past few years that while they were written with good intentions to prevent self-interested patient referrals by doctors, they have incentivized consolidation and impeded care in the healthcare system.
Rightly reformed, these regulations and the safe harbors and exceptions within them, can and should be reoriented to help us transition to a much better kind of healthcare system while still providing the important protections patients and our taxpayer funded programs need.
— Eric D. Hargan (@DepSecHargan) October 9, 2019
HHS Secretary Alex Azar told reporters on a press call that when providers are responsible for outcomes, "you can worry less about micromanaging their incentives, their most powerful incentive will be aligned with their patient's health."
For example, under the proposals, Azar said a dialysis facility or another provider could give patients monitoring technology to allow two-way, real time communication about a patient's condition.
"In addition, the facility could equip the physicians with data analytics software to help them monitor a patient's health outcomes," Azar said. "Physicians could also provide other types of technology for free that could help with chronic conditions, like a smart pill box that reminds a patient when he or she has to take pills, and alerts the physician about missed doses."
One idea sought by the medical device industry, alterations to safe harbors to allow for value-based warranty arrangements, is included in the proposed regulations. But AdvaMed did not get everything it asked for in its comments to the government in October 2018.
"There is not a specific safe harbor for outcomes-based contracting for anybody when you're contracting for the sale of a product, it's really much more when you're participating with others in coordinated care in our rule," an HHS official told reporters. "That said, there is certainly room in the value-based arrangements proposals for many of the constituencies in AdvaMed that deal with technologies in particular."
An HHS Office of Inspector General advisory opinion allowing a device manufacturer to offer a hospital a warranty for a trio of medical devices aimed at reducing readmissions after joint surgery in September 2018 may lend a clue to how device manufacturers will pursue new business opportunities if the safe harbor changes are finalized.
While many of the changes will be welcomed by industry, pharmaceutical manufacturers, durable medical equipment manufacturers and suppliers, and laboratories are excluded from partaking in value-based and patient engagement arrangements, Jennifer Michael, a healthcare attorney at Epstein Becker Green who previously served as chief of the industry guidance branch at OIG, told MedTech Dive in an email. Azar told reporters HHS is still working on separate regulations that would enable value-based outcome payments for pharmaceutical products, and aims to get changes out "as soon as possible."
"The breadth and scope of the proposed new safe harbors is remarkable; unlike OIG's previously issued safe harbors, if finalized, they would protect arrangements of unknown design and unproven efficacy as long as the parties reasonably anticipate the arrangement will advance the coordination and management of care of a target patient population and the arrangement satisfies all of a safe harbor's other requirements," Michael said.
But notably, she added, OIG said in its proposed rule any final safe harbors will only give prospective protection. The proposed rule notes that emerging payment models might present risks that haven't been identified by OIG or the broader healthcare industry.
"Model design characteristics common to properly structured value-based payment models could curb some traditional FFS risks," the HHS OIG proposed rule states. "However, value-based payment models could present other risks, including stinting on care (underutilization), cherry picking lucrative or adherent patients, lemon dropping costly or noncompliant patients, and incentives to manipulate or falsify data used to verify performance and outcomes for payment purposes."
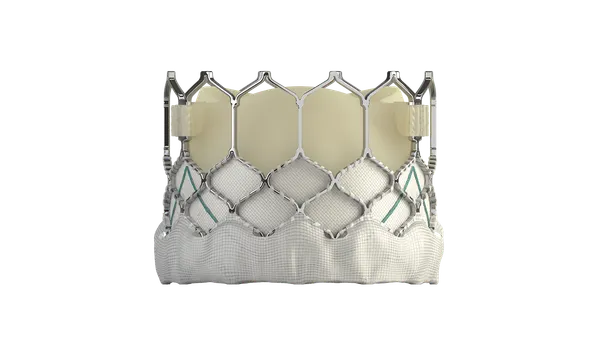
CMS Administrator Seema Verma, White House Domestic Policy Council Director Joe Grogan and Hargan are scheduled to tour a Boston Scientific facility in Maple Grove, Minnesota and host a policy roundtable to discuss the two proposed rules Wednesday afternoon.
Comments on the set of proposed rules are due 75 days after they are formally published on the Federal Register.