Dive Brief:
- The FDA is asking makers of pen needles used for medication injection to review their product labels and training materials after the agency's own analysis of labeling on insulin pens found some manufacturers were not providing clear instructions for use.
- The agency sent a letter to manufacturers making the labeling change request and issued a safety communication for patients, caregivers and healthcare providers that outlines a problem with confusion over how to use pen needles that could prevent a patient from getting their medicine.
- The FDA said it has received reports of patients using standard pen needles to inject insulin without removing the inner needle cover, preventing the insulin from being delivered. Some patients developed high blood sugar because the inner cover stopped the needle from entering the skin, and one patient died after their blood sugar remained too high for too long, FDA said.
Dive Insight:
Confusion can arise when a patient has been taught to use one type of pen needle and then later tries to use another type. The problem may come down to the difference in design between safety pen needles commonly used in hospitals and the standard pen needles patients typically get at home.
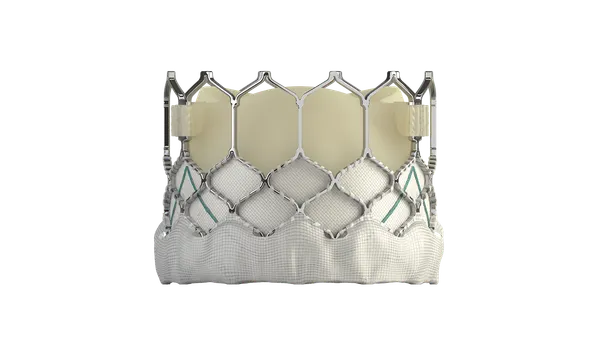
Safety pen needles have a removable outer cover and a fixed inner needle shield that is not removed before an injection. Standard devices for use at home often have an outer cover plus an inner needle cover that must be removed before injection.
Hospitals use insulin pen needles that automatically re-cover and lock the needle once it has been withdrawn from the skin to protect staff from needlestick injuries and to guard against reuse of needles, according to the nonprofit Institute for Safe Medication Practices.
The institute last year issued an alert about the issue of insulin pen misuse after receiving several reports of patients failing to remove the inner cover of a standard insulin pen needle before attempting to administer insulin. In one case, a patient with type 1 diabetes who did not know to remove the inner cover developed ketoacidosis and later died because she had not been receiving any of the insulin doses, the group said.
"Patients using insulin pens with automatic needle retraction devices while hospitalized, but who will be using standard pen needles at home, must be made aware that the standard needle is different. It is imperative that removal of BOTH covers is explained to patients during diabetes education," the institute said in its October 2017 alert.
The FDA asked manufacturers to review their directions for use and training materials to assess whether an update is needed to explain clearly how to use the pen needle and to consider adding a warning in the labeling about the need to remove both the outer and inner needle covers.
Manufacturers should decide whether to make a new 510(k) submission to comply with the labeling change request, the agency said. If no new 510(k) is needed, documentation of the decision-making process and the basis for that conclusion is necessary, the FDA said.
For patients and caregivers, the FDA recommends checking each box of pen needles to see if they are trained to use them, and then seek training if needed. The agency also is asking healthcare providers and educators to take the time to make sure patients understand how to use their pen needles properly and to explain the symptoms of under-dosing of their medication.