Dive Brief:
- FDA will gather its General and Plastic Surgery Devices Panel May 30-31 to seek feedback on the proposed reclassification of surgical staplers for internal use from Class I to Class II, imposing special controls, as well as the reclassification of certain absorbable hemostatic agents from Class III to Class II, the agency announced Tuesday.
- The agency last month disclosed receiving more than 41,000 individual adverse event reports related to surgical staplers and staples between Jan. 1, 2011, and March 31, 2018, including 366 deaths, more than 9,000 serious injuries, and more than 32,000 malfunctions.
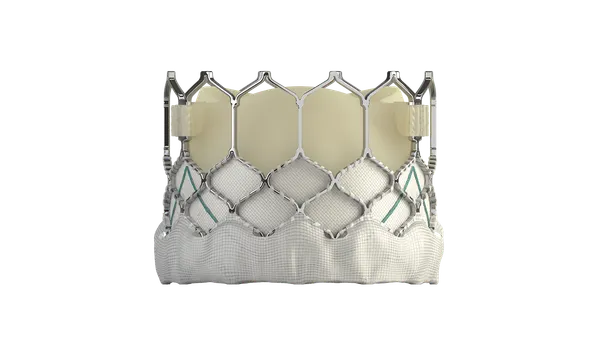
- Separately, the agency scheduled a public meeting of the Circulatory System Devices Panel June 19-20 to address safety concerns surrounding use of paclitaxel-coated balloons and drug-eluting stents in patients with peripheral artery disease, according to an official notice posted Monday.
Dive Insight:
The meetings are the latest in response to a slew of safety concerns surrounding medical devices.
In the case of surgical staplers, a Kaiser Health News investigation shed light on adverse event reports related to the devices that were hidden from public view in alternative databases. FDA alerted healthcare providers to stapler malfunctions a day later.
FDA also released a draft guidance on labeling recommendations for surgical staplers and staples and a proposed rule on reclassification of certain staplers from Class I to Class II, recommending a number of special controls. Malfunction and misuse problems reported with the devices include misfiring of staples, failure of a stapler to fire the staple, and misapplied staples in which incorrect staple size is used for certain tissue.
The possible increase in oversight would also entail distinguishing between staplers for internal versus external uses. FDA defined staplers for internal use as specialized prescription devices used to deliver staples to internal tissues during surgery, which may be indicated for use in gastrointestinal, gynecologic or thoracic procedures.
Conversely, surgical staplers for external uses, like delivering staples to skin during surgery, will remain exempt from premarket review, FDA clarified.
The meeting will be held in Gaithersburg, Maryland May 30 from 10 a.m. to 4 p.m. and May 31 from 8 a.m. to 4 p.m.
As for paclitaxel, a December Journal of the American Heart Association meta-analysis of long-term outcomes in peripheral artery disease patients treated with paclitaxel-eluting stents or paclitaxel-coated balloons prompted FDA to flag a potential heightened mortality risk.
Medtronic, BD and Cook Medical are among the manufacturers that have all since defended the safety of their products.
The advisory panel meeting follows a cautionary letter to healthcare providers last month in which FDA noted the potential for increased long-term mortality associated with the devices. Regulators intend for the Circulatory System Devices Panel to weigh in on the magnitude of the long-term mortality signal and its potential causes, and recommend appropriate regulatory actions.
Coated balloons and stents are used to open obstructions in the femoropopliteal artery. Paclitaxel is released to help prevent formation of scar tissue, which could recreate vessel blockages. The JAHA meta-analysis of 28 randomized clinical trials and a total of more than 4,600 patients raised alarm about the benefit-risk profile of the devices. While researchers found all-cause patient death at one year was similar between patients receiving paclitaxel‐coated devices and control arms, at two years it was "significantly increased" in the paclitaxel group, and up to five years after treatment increased further to a 14.7% all-cause death rate among paclitaxel recipients compared to 8.1% in the control group.
"Further investigations are urgently warranted," the JAHA researchers concluded, leading FDA to notify healthcare providers in January it was evaluating the issue.
The FDA then in March reported its own preliminary analysis of long-term follow-up data, finding "a potentially concerning signal" of increased long-term mortality in study subjects treated with paclitaxel-coated products, namely an approximately 50% increased risk of mortality in subjects treated with paclitaxel-coated devices at five years.
FDA noted the data "should be interpreted with caution" due to limitations in the long-term data and because the specific cause and mechanism of the increased mortality are unknown.
The agency encouraged providers to consider the findings when making treatment recommendations and facilitating the informed consent process, and also advised use of alternative treatment options until further studies have been conducted. Still, FDA noted that in patients at particularly high risk for restenosis, the renarrowing of an artery, providers may determine the benefits of using a paclitaxel-coated product outweigh the risks.
The meeting will be held in Gaithersburg, Maryland June 19 from 8 a.m. to 5 p.m. and June 20 from 8 a.m. to 3 p.m.