Metal implant manufacturers may soon face more stringent labeling requirements if U.S. health regulators follow advice laid out by its Immunology Devices Panel this week.
FDA convened the group of experts to help lay a foundation for examining how and why some patients have adverse allergic and immune responses to materials commonly used in medical devices. Widespread problems with much-litigated devices like corrosive metal-on-metal hip replacement systems and Bayer's birth control device, Essure, were initial sources of public pressure for FDA to consider patients' relationship with metals.
A number of public speakers who suffered adverse responses to implants told regulators about exceedingly difficult attempts to track down ingredients lists for their devices — information that could be critical to predicting or better understanding poor experiences with medical technologies.
"It would be beneficial to get a listing of the specific elemental composition of these devices included on the packaging," panel chair Raj Rao, head of orthopaedic surgery at George Washington University, said on behalf of the advisory group.
When pressed to clarify what labeling specifics companies are currently required to include with a device, and whether regulators ever do testing to verify those claims, Jennifer Goode, biocompatibility program advisor in the Center for Devices and Radiological Health, said FDA does "not commonly require" manufacturers to disclose the level of detail Rao described.
Panelist Whitney Christian, a toxicologist at Medtronic, said industry supports patients' and doctors' "right to know" what's in devices and is willing to work with FDA on the issue. The sentiments echoed those of AdvaMed representative Susan Alpert, previously chief regulatory officer at Medtronic, who similarly expressed manufacturers' interest in the materials conversation.
"There are people who can't receive the benefits because of the materials we've chosen," she said in comments Wednesday, noting that manufacturers need to communicate more effectively with those individuals so they have the option to choose a different, better-suited therapy.
FDA's Aron Yustein, assistant director of clinical and scientific policy staff in the Office of Product Evaluation and Quality, said such a change in labeling expectations for manufacturers of metal devices could mirror similar pushes for ingredient transparency in other realms of medical device regulation.
"We've heard that from the public on other areas too," he said, calling attention to a similar push from breast implant safety advocates. In late October, regulators followed up on a March advisory committee meeting with a proposal that ingredient information not just be included in FDA's summary of safety and effectiveness data posted online, but also in patient labeling.
Many culprits
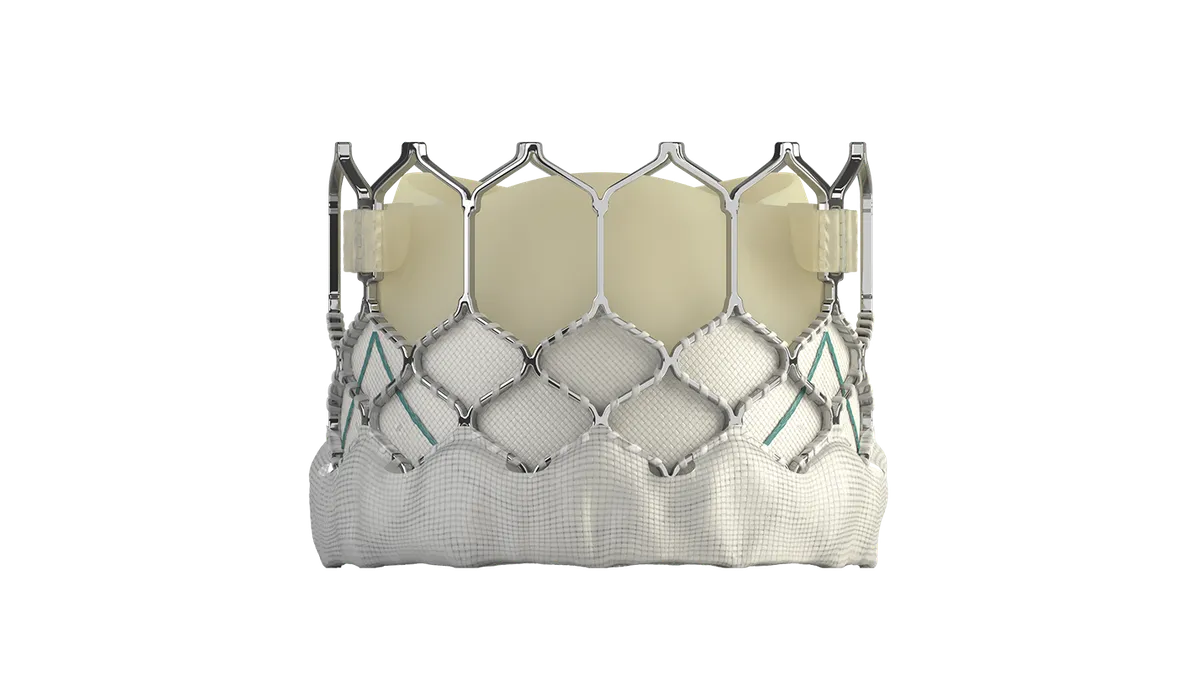
Public speakers were quick to highlight examples of adverse events tied to metal-containing implants across a broad spectrum of medical devices. Among them: copper IUDs, spinal fusion devices, and metal clips and staples used in surgery.
"The news to the panel is: This is a common problem," said Stephen Tower, an orthopaedic surgeon who has studied health outcomes in recipients of chrome and cobalt hip components.
Concerns over harmful metal corrosion led industry to shift away from metal-on-metal artificial hip systems and create other modular systems involving ceramic and polymer materials in conjunction with metal. But Tower said he continues to see individuals having problems with many popular hip designs still commonly implanted. "This is not a metal-on-metal problem," he told the panel.
A data analysis presented by Madris Tomes, a medical device adverse events and unique device identifier expert, showed reports filed to FDA citing autoimmune and allergic reactions span a range of devices with various combinations of metal, ceramic and polymer materials.
Tomes also called attention to dental implants, which with more than 2.2 million adverse event reports sent to FDA make them the second most implicated category of devices, she said. Of those reported issues, more than 95% were only made publicly available once FDA shared alternative summary reports earlier this year — an overwhelming data dump, Tomes described. "I had to back down because Microsoft Excel is not that big," she said.
She urged FDA to inform healthcare providers via a Dear Doctor Letter of awareness of systemic, albeit poorly understood, issues related to metal-containing devices, noting that FDA's advisory committee meetings often generate new public awareness around safety issues and lead to a spike in adverse event reporting.
We need more research, but how?
Aside from recommending FDA implement more transparent labeling, the meeting ended with few clearly laid out action items.
Participants agreed on the importance of extensive further research into the mechanisms behind disparate reactions, and which implant and patient factors increase likelihood of poor outcomes. But beliefs on the best ways to gather useful data varied.
Panelist Joshua Jacobs, an orthopaedic surgeon at Rush University who has accepted consulting fees and other payments from Zimmer Biomet and Medtronic, said that leveraging joint replacement registries will be important, but creation of a national implant retrieval registry to study failed implants and surrounding tissues would be even more impactful.
"Implant retrieval programs already exist in several centers ... it's hard to fund them, they're hard to support, and yet we get tremendous information from them," Jacobs said. "That's a resource I encourage us to develop ... to get some really basic answers."
Another panelist, Cedars-Sinai Medical Center rheumatology chair Michael Weisman, advocated for a longitudinal cohort study of at-risk patients. But other members of the panel noted that trying to learn from isolated incidents may be a better use of resources.
At least one expert tempered near-term expectations on FDA's goal of supporting development of tests to better predict patients' responses to metal implants. Given the lack of understanding of underlying biological mechanisms, "we're a long long way from being able to do that well," said biostatistician Jason Connor.
Until then, identifying and attending to individuals who have problems with implants as quickly as possible is "the most patient-centric thing we can do."
"Mitigate is the key word here," Connor said.
Rao affirmed the lack of new insight on near-term solutions on pre- or post-surgery immune response testing. "I don't think the panel has any additional new information at this point to recommend to FDA," he said.
In the meantime, some panelists suggested healthcare providers can do a better job informing patients about what the medical community does and doesn't know about potential immune reaction risks with metal implants. For example, it might be worthwhile to ask patients about family history of autoimmune disease, which some people believe may increase risk for a heightened reaction to introduction of an implant.
Panelist Stephen Badylak, a University of Pittsburgh surgeon and regenerative medicine expert who has accepted funds from C.R. Bard, shared that sentiment.
"When I hear about patients who have had a problem [because they weren't informed] ... I don't want to say it's a crime, but it probably should be."