Dive Brief:
- Exact Sciences shared early results of a test it is developing with Mayo Clinic to screen for esophageal cancer and its precursors.
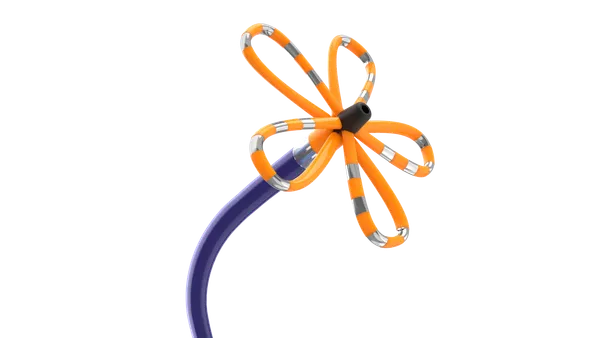
- The test, called Oncoguard Esophagus, uses an encapsulated sponge device to collect esophageal cells. DNA is extracted from the cells and processed in a PCR assay. The results from the assay are run through an algorithm, which provides a positive or negative result, Paul Limburg, Exact Sciences’ chief medical officer of screening, wrote in an email.
- The test, which is designed to be less invasive than an endoscopy, detected esophageal adenocarcinoma and Barrett’s esophagus, a known precursor to the cancer, according to results published in Clinical Gastroenterology and Hepatology. The National Institutes of Health and Exact Sciences funded the study.
Dive Insight:
Esophageal adenocarcinoma is the most common form of esophageal cancer in the U.S. It typically has no early symptoms, so it is often diagnosed in the later stages.
Barrett's esophagus, a condition where the cellular structure of the esophagus lining changes due to irritation, can sometimes progress to esophageal cancer.
Currently, an endoscopy is the gold standard for screening for esophageal cancer and Barrett’s esophagus, but it can be expensive and inconvenient.
“Standard methods of screening can be invasive and costly for patients, which is why there has been a recent push to change the screening guidelines to include non-endoscopic tests,” Prasad Iyer, a professor of medicine in gastroenterology and hepatology at Mayo Clinic Comprehensive Cancer Center, said in a statement.
Exact Sciences worked with Mayo Clinic to develop a less-invasive screening method for esophageal cancer and Barrett’s esophagus. The Madison, Wisconsin-based diagnostics company is known for its noninvasive Cologuard screening test for colon cancer.
The companies shared published results of the new test on Thursday. Esophageal specimens were collected from 352 people for an algorithm training set and 125 people for a test set using the sponge collection device. The samples were then assayed for methylated DNA markers. The patients later underwent an endoscopy.
Results from the test set found 88% sensitivity at 84% specificity for detecting Barrett’s esophagus, and 100% sensitivity for detecting esophageal adenocarcinoma and Barrett’s esophagus with high grade dysplasia.
Exact Sciences also said the sponge collection method was well tolerated and could be used in an office setting. When asked a week later, the majority of patients said they would undergo the collection procedure again if indicated.
Exact Sciences is doing further work to develop the test, including studying the assay using the locked algorithm in a primary care population in Minnesota and Wisconsin. The next steps are clinical validation, including validation of the laboratory where the test will be run, Limburg said.