Dive Brief:
- Intrinsic Therapeutics has received FDA premarket approval for its Barricaid annular closure device used in spinal surgery to prevent recurrent disc herniation.
- The authorization comes more than a year after an FDA advisory panel, by a 9-5 vote, recommended against approving the device based on safety concerns. That panel also voted 12-1 in favor of the effectiveness of the device.
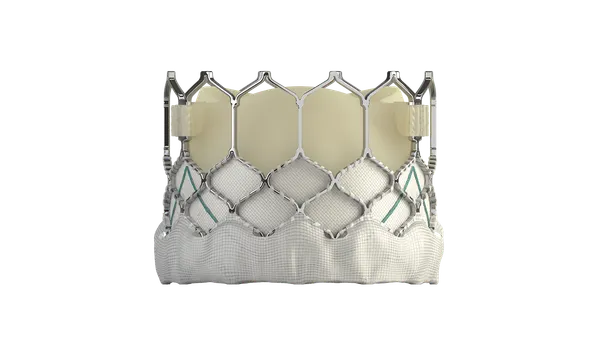
- Barricaid is designed to close large defects in the annulus, the tough circular exterior of the intervertebral disc, allowing the surgeon to preserve more of the patient's disc, according to the company's website.
Dive Insight:
The device is intended to prevent re-herniation of the disc. It consists of a woven polyester occlusion component intended to block the annular defect while anchored to the adjacent vertebral body by a titanium bone anchor.
A two-year clinical trial of 550 patients published in The Spine Journal found the device compared to standard treatment was statistically superior on all endpoints, including recurrent herniation and a composite of patient reported outcomes.
Those results appeared to satisfy regulators after an earlier thumbs down from FDA advisers.
In December 2017, FDA's orthopaedic and rehabilitation devices panel voted in favor of the device's effectiveness but expressed concerns about its safety, focusing on a high percentage of end-plate lesions in Barricaid patients compared to control patients in a clinical trial. The panel said it was unclear what the lesions represent, according to a summary of the meeting.
The panel had additional concerns with long-term safety, and said the study's statistical methodology may not provide a complete picture of long-term outcomes.
In May 2017, Intrinsic Therapeutics announced it closed a $49 million financing round consisting of $28 million in equity co-led by New Enterprise Associates and Delos Capital and a $21 million debt facility with CRG.
In announcing the funding round, Intrinsic said it filed its PMA application with FDA in December 2016, based on the outcomes of a two-year, multi-center prospective randomized superiority trial of 554 subjects at the greatest risk of re-herniation and re-operation.
Lumbar discectomy is a common operation performed to treat lower back pain. When the annulus is damaged, the soft inner part of the disc bulges out. The herniated disc can press on the spinal cord and cause pain, tingling or weakness in the back or legs.
In the discectomy procedure, a surgeon takes out part of the damaged disc to ease the pressure on the spinal cord. Patients with large annular defects, however, run the risk of the disc becoming re-herniated. In a recent study of 253 patients who underwent a limited discectomy, 25% experienced symptomatic recurrent lumbar disc herniation. Of those 64 patients, 36 underwent a subsequent surgical procedure.