Telehealth advocates are looking to capitalize on virtual care’s positive momentum after two years of COVID-19, hoping to shape a friendlier physician licensing landscape as states increasingly reformulate policies mediating cross-state care.
But there’s a complication: No one solution to the U.S.’ patchy physician licensing infrastructure has universal buy-in from the telehealth industry.
Some groups push for greater state adoption of compacts like the Interstate Medical Licensure Compact, which makes it easier for doctors to obtain licenses in bulk from the 38 participating states. Others lobby for reciprocal licensure arrangements between the states.
Telehealth stakeholders are also split on the role that the federal government should take.
The licensing of medicine is a state determination, though some are hopeful Washington could step in and open the doors to cross-state practice, which the nation was able to temporarily sample due to more generous licensure policies during COVID-19 that states are now rolling back.
Virtual care advocates say opening up cross-state care is integral to patient access moving forward. However, it’s unclear how much effect expanding cross-state telehealth access would have.
Though telemedicine across state lines increased significantly amid pandemic waivers, it still made up a small portion of overall Medicare telehealth usage, a recent study in Health Affairs found.
Out-of-state visits represented 5% of all virtual visits in 2020 and 0.8% of all outpatient visits. That’s compared with 8% of all virtual visits and 0.1% of all visits between 2017 and 2019, the University of Michigan researchers found.
Despite the small incidence, rural patients were more likely to use virtual care between states, suggesting its usefulness for expanding access to patients with geographic barriers to care. And, though most states saw fewer than 1% of overall visits virtually across state lines, utilization varied widely across the U.S., leading researchers to suggest decisions that future telehealth access is best left up to the states.
“In a short period of time the conversation has changed,” said Kyle Zebley, VP of public policy for the American Telehealth Association and executive director of ATA Action, a unit of the ATA focused on lobbying state and federal government to permanently enact temporary COVID-19 telehealth flexibilities. “There’s a lot of data that we can go back to and point to and say this worked.”
States: the starting line
The fact that medical licenses are granted and managed by state medical boards is a “complicating factor, to say the least, for the delivery of care across state lines,” Zebley said. “Prior to the pandemic, this was unquestionably a hindrance.”
Telehealth licensure prior to the COVID-19 pandemic was largely based on three models: being licensed in and caring for patients in a state; being a member of a licensure compact that allowed for care between states; or specific and prescriptive temporary licenses for telehealth. However, cross-state practice was uncommon, according to Latoya Thomas, senior director for policy and government affairs at virtual care company Included Health.
During COVID-19, states — needing doctors to help overwhelmed hospitals and facing a rising demand for telemedicine — enacted temporary allowances for clinicians who were properly licensed by another state to deliver services.
During the height of the public health emergency, all 50 states and Washington, D.C. used emergency authority to waive at least some aspects of their state licensure requirements.
But as the public health response to COVID-19 winds down, more and more states are ending their waivers or allowing them to expire, resulting in millions of patients losing that expanded access to telehealth.
As of mid-April, 15 states still had licensure flexibilities in place, down from 24 in early March, according to a tracker maintained by telehealth lobbying group the Alliance for Connected Care.
In many of the remaining states, cross-state licensure flexibilities are set to expire this summer, or are tied to the duration of the federal public health emergency.
The loss of those waivers will impact care for patients who began seeing out-of-state providers during the pandemic, telehealth advocates say.
“I certainly see this being a precursor to some sort of stagnation for patients,” Thomas said.
It could also affect the ability of providers to fill demand for healthcare services remotely, which could compound issues like burnout and provider attrition creating that are creating staffing shortages in many pockets of the U.S.
Telehealth is a “load-balancing infrastructure,” said Roy Schoenberg, CEO of telehealth company Amwell. COVID-19 was one example of telemedicine’s usefulness in an emergency, but remotely based doctors could be helpful in other disasters, like floods in Houston or fires in California, according to the executive.
“We have all the clinician resources we need. We just can’t mobilize them because of red tape,” Schoenberg said.
Before COVID-19, there was little action to facilitate cross-state care for a number of reasons. For one, public demand for telemedicine was low. Proponents of state medical boards, which issue licenses and oversee doctors, argued allowing more cross-state medical services could impact physician quality and patient safety.
In addition, state medical boards have significant financial incentives to retain the current licensing system, as a notable share of their revenue comes from license application and maintenance fees.
For example, California’s medical board brought in $56 million — 91% of its total revenue — last year from physician renewals and application fees.
“States are looking at their balance sheets,” Thomas said. “By waiving licensure waivers it does impact revenue.”
Compacts and recognition
Adoption of interstate compacts allowing for care between states has exploded over the past decade, expanding from the Nurse Licensure Compact, which allows nurses to practice in other participating states without having to obtain additional licenses, to more recent iterations for doctors, counselors, physical therapists and other practitioners.
Many in the telehealth industry think the most expedient path forward to facilitating cross-state care is to nudge more states to adopt compacts.
“At this point, the only feasible pathway forward is for states to join existing cross-state compacts,” Thomas said. “It’s not perfect, but at least you have some uniformity you can expect with respect to licensure. Presently, we just don’t have that.”
Specifically, the Interstate Medical Licensure Compact, which had its 38th state sign on in May, is supported by the American Medical Association and the Federation of State Medical Boards, which represents U.S. medical and osteopathic boards.
The IMLC allows for a streamlined application process, making it easier for clinicians to apply en mass for licenses. However, it doesn’t change the underlying licensing structure.
It also doesn’t allow for reciprocity, so isn’t a silver bullet for telehealth vendors looking to get their doctors licensed across the U.S.
“You still have to apply and pay and satisfy the requirement of each medical board in the state you want to practice,” Schoenberg said.
Amwell uses the IMLC to get its Amwell Medical Group clinicians licensed in multiple states. It’s a time-consuming and expensive process — Amwell has a whole department dedicated to getting its more than 6,500 in-house doctors multilicensed.
Typically, Amwell sees average licensing costs of about $1,000 per state, which comes out to roughly $50,000 per provider for nationwide practice. Renewals are required every two to three years, and usually cost about half of the initial fee, the company told Healthcare Dive.
“It’s a mess. There’s no way around it. If a clinician wants to be available in every state they need to go through the same path as if they lived in every single state,” Schoenberg said.
Additionally, a number of states haven’t joined existing compacts, including states with large patient pools like California and New York.
States that haven’t joined often have vocal labor groups and many in-state doctors that have expressed reservations about the compacts. Though interest seems to be growing: New York, North Carolina, Virginia and Indiana are just a handful of states with active bills in their state legislatures to join the IMLC.
"It's a mess. There's no way around it."

Roy Schoenberg
Amwell CEO
“The Interstate Medical Licensure Compact is something that we are supportive of and we urge states to adopt it because its an improvement on the status quo,” ATA’s Zebley said. “However respectfully — respectfully — we think a reciprocal licensure arrangement is our preference.”
Under a reciprocal licensure arrangement, states would mutually recognize medical licenses granted by other states, like in the Nurse Licensure Compact. Physicians would be held accountable for care in the state where the patient is located.
Such arrangements could be adopted by state legislatures, and are supported at least in part by the Federation of State Medical Boards.
Recently, the FSMB updated its telemedicine policy for the first time in nearly a decade. The policy includes suggested exceptions where states could allow care across state lines provided by a physician licensed in another state, including for follow-up care, patients in transit or second opinion consultations.
The FSMB document is nonbinding, but past iterations have been used widely by state legislators, regulatory agencies and medical boards to craft telehealth policies, according to Zepley.
“Lots of areas just make common sense,” Zepley said.
Federal role
Despite the federal government having no direct licensing authority, some members of the telehealth industry see areas where Washington could take a more active stance.
One of the most important things the federal government could do in the near term is make it clear that streamlining cross-state care is a national priority, and take an active role in determining which carrots and sticks it thinks are best, argued Amwell’s Schoenberg.
The government could tie federal funding to states that adopt compacts or enact reciprocal licensure arrangements, or mandate automatic reciprocity. That’s already the case for the Veterans Affairs health system, where any employed doctor, no matter where licensed, can provide virtual care to any VA patient, no matter where located.
Telehealth researcher Ateev Mehrotra supports building on that strategy. Mehrotra argued in a New England Journal of Medicine perspective last year: “Perhaps the most promising strategy is one that uses federal authority to encourage reciprocity ... Physicians could be permitted to provide telemedicine services to Medicare beneficiaries in any state, as long as they possess a valid medical license.”
“Such a policy would most likely accelerate the adoption of state legislation regarding reciprocity, thereby affecting patients with other forms of insurance as well,” Mehrotra continued.
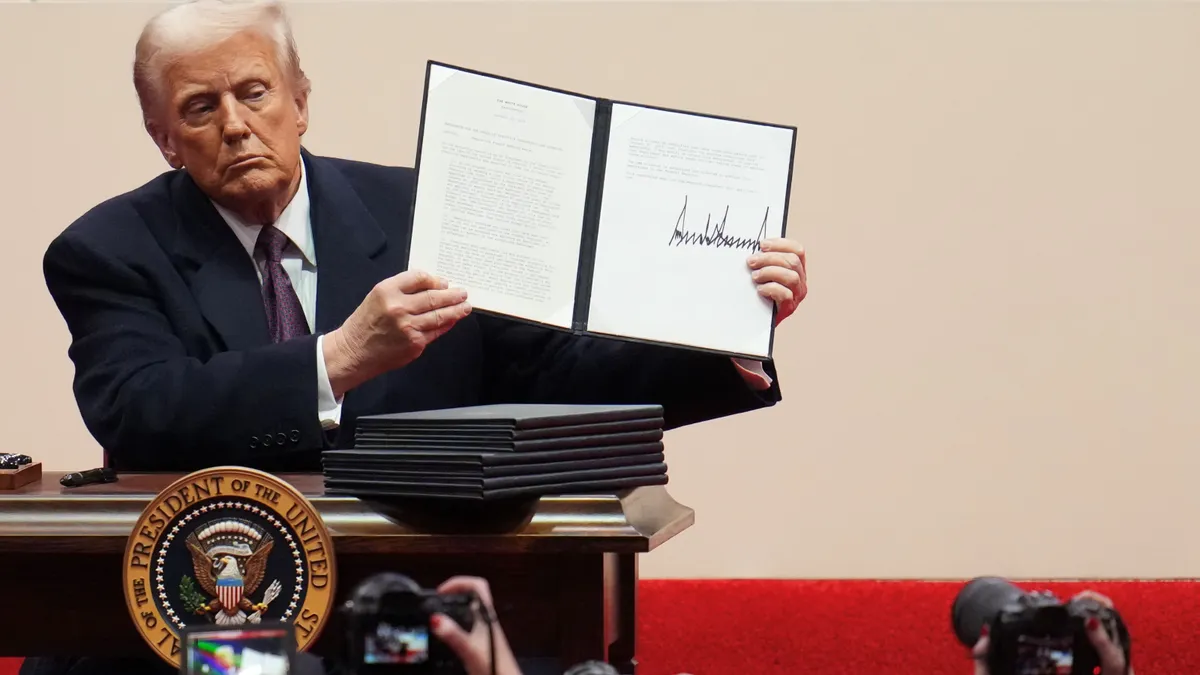
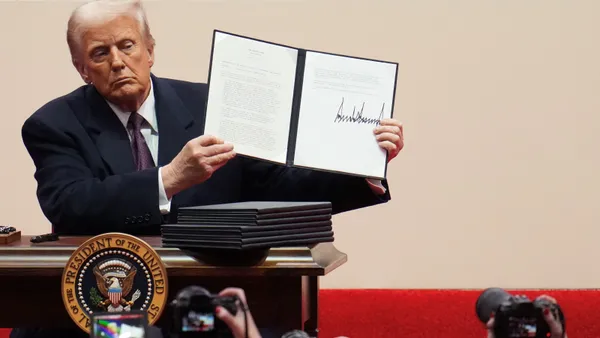
Though the Biden administration has noted it’s eager to foster telehealth, there doesn’t appear to be broad support in Congress or the White House for such a sweeping change to how the U.S. licenses its doctors, even just for telemedicine.
Two recent bills have been proposed to revamp cross-state licensing for telehealth, but neither has made it past committee.
One introduced by Rep. Ted Yoho, R-Fla., would make funding from the Bureau of Health Workforce contingent on adopting the IMLC within three years. The other, introduced by Sens. Ted Cruz, R-Texas, and Marsha Blackburn, R-Tenn., would temporarily authorize a provider licensed in one state to provide telemedical care to patients in other states, but only during the COVID-19 emergency.
Given federalism, it’s highly unlikely that Washington will preempt state law. And with patchwork, state-by-state laws governing the practice and provision of medical care, there isn’t a one-size-fits-all solution for cross-state care, experts said. That brings the discussion back to the states.
“At the end of the day, for political and constitutional reasons, I think you’re still going to have to convince state legislators that it’s in their best interest and the best interest of their constituents to adopt,” Zepley said.