Dive Brief:
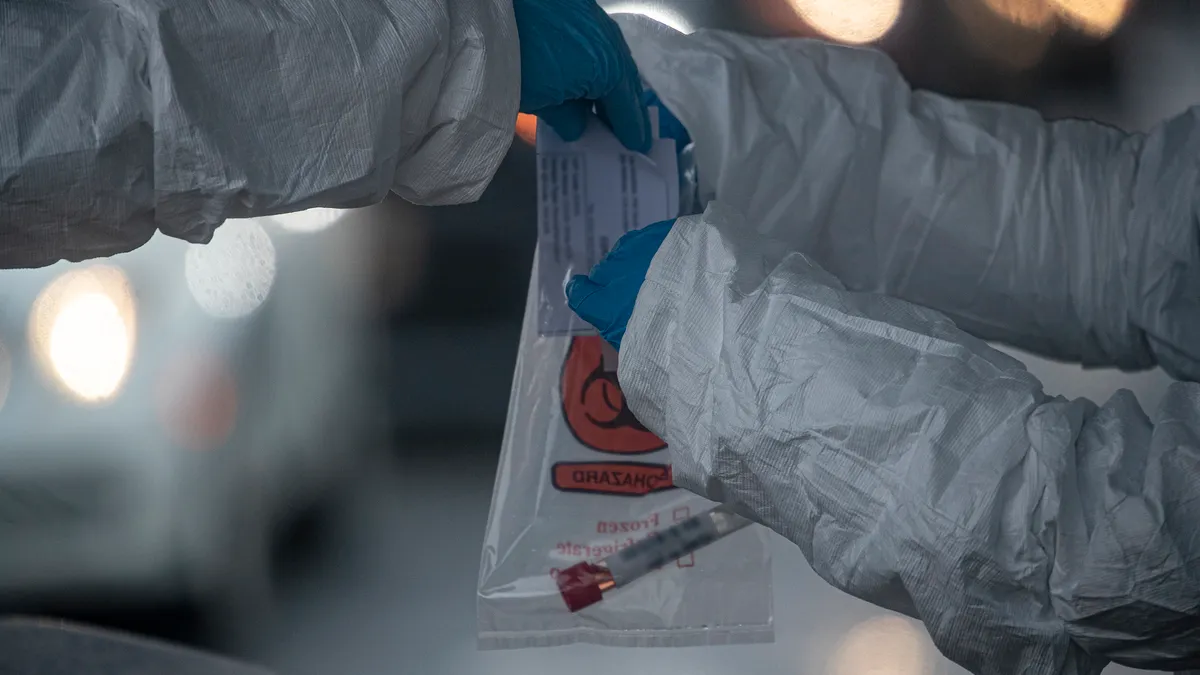
- Diagnostic testing for COVID-19 will cost an estimated $6 billion to $25.1 billion annually, while antibody testing costs could range between $5.2 billion and $19.1 billion, according to a report by Wakely Consulting Group commissioned by America's Health Insurance Plans.
- The large variance is due to uncertainty as to which type of test will be used most along with the unknown future level of testing and variability in costs per test. The higher estimate assumes a scenario of widespread, higher-cost testing, like those for returns to work and school, the report published Wednesday said.
- The estimated costs for administering the tests were between $95 and $130 for diagnostic testing for Medicare and Medicaid and between $90 and $125 for antibody testing, depending on location. Commercial administration was counted at about 25% higher.
Dive Insight:
As the United States begins the difficult process of reopening, public health experts agree widespread testing is a key component of safely returning to more normal activities.
But the country has struggled to get diagnostic efforts off the ground, with several missteps from the Centers for Disease Control and Prevention along with a largely uncoordinated federal response.
Commercial players have stepped in with diagnostic and antibody tests that FDA has authorized for emergency use, but many still have been dogged by accuracy concerns.
Meanwhile, the question of how the tests will be paid for as availability and need ramps up has been muddled.
The Coronavirus Aid, Relief, and Economic Security Act passed in March requires insurers to cover all tests without cost-sharing, but only if a provider determines it medically necessary. That would exclude precautionary testing such as for employees returning to an office not showing symptoms.
While hospitals have pushed for private payers to do more to help them deal with the pandemic and its associated costs, AHIP has maintained the sector is doing enough. Major payers have all waived cost-sharing for COVID-19 treatment as well as testing and many have expanded telehealth reimbursement and rolled back prior authorization requirements.
AHIP said in a statement Wednesday guidelines for widespread testing — and how it is paid for — should be made more clear.
"Testing strategies need to be part of a holistic public and occupational health strategy," the group wrote. "Federal guidance should consider funding for testing in that context, and should clearly articulate the roles of insurance providers, employers, and public health officials."
So far, big payers have weathered the COVID-19 crisis with little impact to their bottom lines as hospitals put off pricier elective procedures. But as non-emergency care is restarted, that could change.
A separate AHIP report published earlier this week estimated that costs for treating COVID-19 this year and next could reach $200 billion, not including testing or accounting for deferred care. And actuaries in California warned in March that plans in the individual marketplace could see premium rates increase by as much as 40%.