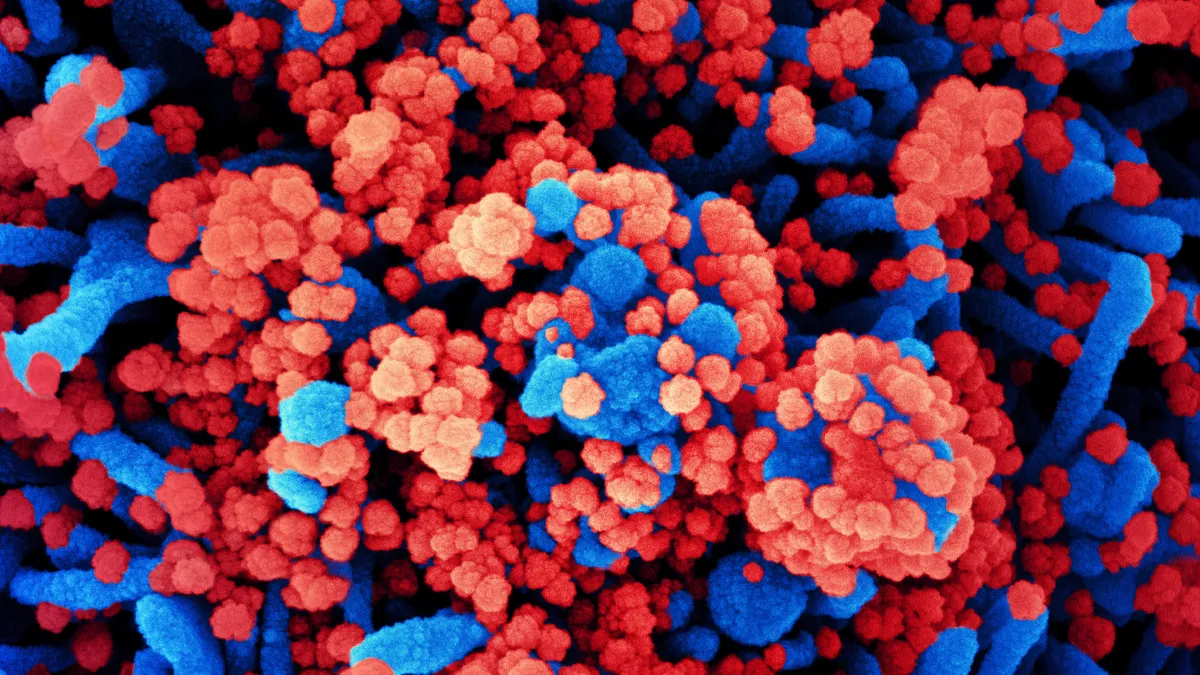
Viruses are shape-shifters, naturally mutating as they go up against the immune defenders of their hosts. This forced evolution is why the influenza vaccine must be updated annually and one reason why no successful shot for HIV has been developed.
Coronaviruses like SARS-COV-2 mutate more slowly than either of those viruses. But changes to their genetic code inevitably accumulate, with the chance that some may affect their infectiousness, lethality or resistance to vaccines. That appears to now be playing out with SARS-CoV-2, as the emerging variants identified in the U.K., South Africa and Brazil seem to spread more easily.
So far, however, the available evidence doesn’t indicate the new variants can evade either of the vaccines developed by Pfizer and Moderna, a fact which has many public health experts urging calm.
"What you really care about is vaccines. Vaccines are our way out of this," said Paul Offit, director of a vaccine center at the Children’s Hospital of Philadelphia. "If you start to see people who have been vaccinated getting admitted to the hospitals, that’s when you worry."
Nonetheless, some drugmakers are starting to make adjustments that could help them stay one step ahead of SARS-CoV-2’s evolution. Moderna, for instance, plans to test a three-shot regimen of its vaccine, after laboratory evidence showed the immune response stimulated by its shot is weaker against the South African variant. The third shot would come six to 12 months after the second, Moderna said.
"The most straightforward way to raise somebody's [immunity] is to just give them another booster shot," said Tal Zaks, Moderna’s chief medical officer.
Moderna is also developing a booster shot specific to the South African variant, which could be employed as the second injection of a two-dose regimen. On Wednesday, Pfizer and partner BioNTech released data from a laboratory analysis of their vaccine’s response to mutations in the South African variant, which the companies said had only a small effect on its potency.
Even so, using laboratory tests to understand how well vaccinated people will be protected from new variants is an "imperfect" science, Offit noted.
Other companies are rising to the challenge. Gritstone Oncology is preparing to test in humans coronavirus shots that it hopes will stimulate a stronger response from virus-fighting T cells, in theory offering broader protection against multiple types of coronaviruses. Eli Lilly, Vir and GlaxoSmithKline, meanwhile, are testing combinations of man-made antibodies that could be used to treat or prevent infection from a wider array of variants.
'Evolution is unforgiving'
Coronaviruses mutate more slowly than other so-called RNA viruses — such as influenza, HIV and hepatitis C — because they have a "proofreading" function to correct errors as they replicate in cells. This function is necessary because SARS-CoV-2 and other coronaviruses have a longer genome to copy, said William Petri, an infectious disease professor at the University of Virginia medical school.
But due to the extensive spread of SARS-CoV-2 around the world, mutations are piling up, resulting in more distinct variants.
"What we’re seeing is a reflection of millions of people being infected, so that even with a slow mutation rate, evolution is unforgiving," Petri said. "You’re going to see a selection of viruses that transmit more quickly than those that transmit more slowly."
And with faster spread, vaccination campaigns become even more urgent, as do other measures like masks and social distancing, he added.
"With more transmissible variants that means higher levels of herd immunity are going to be necessary," noted Petri. Rather than 70% of the population needing immunity, the number could be as high as 90%, he said.
The South African variant, known formally as B.1.351 has raised particular concerns, because of the number of mutations from the original variant that emerged in China, as well as the way those alterations affect its interaction with antibodies.
In the virus’ characteristic "spike" protein, which both Pfizer’s and Moderna’s vaccines target, B.1.351 has 10 amino acid changes. Importantly, three are on the top of the protein, an area called the receptor binding domain. This is where the virus interacts with and gains entry into cells, but also where antibodies bind most effectively, Stephen Hoge, Moderna’s president, said in a Tuesday presentation.
As a result, Moderna’s vaccine, which was shown to be 94% effective in preventing COVID-19 in a large clinical trial, doesn’t appear to be as potent against B.1.351. Tested against a man-made "pseudovirus" based on the variant, blood samples taken from vaccinated study participants generated six-fold lower levels of neutralizing antibodies. But because the immune response triggered by the vaccine is so strong, Moderna expects the shot will still be protective even after accounting for the reduced antibody activity.
"The good news is that the level of neutralizing [antibodies] that we saw in this [test] suggests to us that we are still effective in being able to protect against the South African strain of the virus that’s now circulating," Hoge said.
Pfizer and BioNTech’s analysis, by comparison, did not find much difference in antibody response between the original virus and the South African variant. But the pseudovirus the companies created for its test had only three of the amino acid changes that were distinctive to the variant, not all 10.
Additionally, the analyses done to date to measure vaccine effectiveness against the newer strains have only looked at antibody levels, Offit pointed out, not other components of immunity like white blood cells, which may mean the vaccines will still remain effective.
Moderna’s plan to study a revised booster shot and a three-dose regimen, however, is part of an ongoing strategy to adjust to the realities of the disease, according to Hoge. "It's important that we may remain vigilant and develop potential tools and countermeasures that would allow us to continue to beat back the pandemic," he said.
Moderna’s vaccine uses genetic material called messenger RNA to instruct cells to produce the spike protein, which in turn stimulates a protective immune response. That mRNA sequence, though, can be quickly changed to account for amino acid changes — the original sequence used, for example, took two days to finalize. And BioNTech executives have said they can design an updated shot in four to six weeks.
A redesigned booster shot could likely gain FDA clearance on the basis of trials in a few hundred people to confirm it’s safe and spurs an immune response, agency officials have suggested. The process might look similar to what happens with seasonal flu vaccines.
A large trial involving thousands of participants would be impractical in any case because it would require specific testing for the South African variant.
One remaining challenge, however, is the lack of clear data about what minimum level of immune response correlates to disease protection. Petri, however, believes that data could soon be available as researchers study blood samples from immunized people who got sick between their first and second vaccine doses.
Adaptation could prove to be a bigger challenge for other types of shots, such as the viral vector vaccines that Johnson & Johnson and AstraZeneca are developing. In those candidates, the genetic engineering necessary to encode for the South African strain is more complex, Petri said.