The lack of a nationwide health IT infrastructure is making COVID-19 case reporting disjointed and duplicative, hamstringing the response to the pandemic, according to U.S. public health experts and commercial labs.
Overlapping local, state and federal government reporting requirements, lack of lab funding, a patchwork electronic reporting system and incomplete patient data is stopping public health agencies from getting a holistic picture of the pandemic, even as the Trump administration says it may reopen the economy in a matter of weeks.
Allowing businesses to open their doors and Americans to flood public areas without the proper reporting infrastructure is likely to lead to a resurgence in coronavirus cases, epidemiologists say. Myriad private stakeholders have proposed plans for such a network and the White House is reportedly exploring the idea. But the administration has taken few concrete steps to patch the health IT holes in its coronavirus response — holes leading to COVID-19 cases being significantly underreported, experts say.
Commercial labs are sending COVID-19 test results directly to the Centers for Disease Control and Prevention in accordance with the Coronavirus Aid, Relief, and Economic Security Act rescue package. Labs also have to comply with a variety of state and federal reporting laws, all while fielding separate requests for data from state health information exchanges, governor's offices, Medicaid plans and government contractors, among other bodies.
Labs are concerned these overlapping reporting goalposts will create duplicate testing and diagnostic results, throwing off any attempt at centralized COVID-19 tracking.
"We've responded to multiple requests from different states for different cuts of data output," Tom Wagner, a VP at lab giant Quest Diagnostics, said Wednesday at a virtual meeting of health IT congressional advisory group HITAC. "The leaders are at their best when they connect on a complete picture, and providing that picture should be much, much easier."
The American Clinical Laboratory Association, which represents Quest and LabCorp, among others, says its members have performed more than 2 million COVID-19 tests since FDA expanded guidance in late February. But requirements from multiple levels of government are throwing a wrench in the testing and reporting process and slowing testing ramp-up, Liz Thomas, ACLA's director of government affairs, said.
Along with the lack of a centralized system for the data, public health agencies are receiving information in different file formats that have to be processed separately, further straining the system. That's when data is received electronically at all — many provider case reports come in a PDF file sent to a CDC email address or even via fax, according to a recent Health Affairs blog.
"Public health is spending time digitizing the information, rather than being able to immediately analyze and act upon it," said Janet Hamilton, executive director of the Council of State and Territorial Epidemiologists.
CDC is scrambling to automate the reporting process so that data in provider EHRs can be sent directly to public health agencies. The agency is currently working on a FHIR-based app to connect COVID-19 electronic case reporting to existing health IT infrastructure to confirm cases and route the data to appropriate end users, with an expected launch date in early May.
But many COVID-19 cases, when reported, are missing critical data like demographic or contact information, public health agencies say. That leads to delays in contacting positive patients, confirming diagnoses and beginning contact tracing — a critical step before the government should even consider re-opening the economy.
Despite a slowdown this week, testing volume has ramped up over the past month, public health experts and lawmakers are growing increasingly frustrated by the piecemeal data being collected. Labs often receive incomplete patient information from providers, and since labs typically don't interface directly with patients — specimens are usually collected in a hospital, doctor's office or drive-thru testing site — it's hard for them to fill in the blanks.
Labs only see the patient directly about 40% of the time. "Knowing who our patient is is based on the data given by the order provider about 60% of the time, and in this pandemic, knowing is critical," Quest's Wagner said.
According to the Council of State and Territorial Epidemiologists, states say once COVID-19 data finally reaches them, the demographic information of race and ethnicity is missing 85% of the time and patient address is missing half of the time, handicapping research and contact tracing efforts.
"Obviously, we can't locate or call someone if we don't have that," CSTE's Hamilton said.
Demographic data is especially important as researchers have found African Americans and other non-white populations are much more likely to contract and die from the coronavirus, according to states with racial data available.
Democrats have introduced a bill that would require HHS to collect and report racial and ethnic data related to COVID-19. The bill benchmarks $50 million to help with the effort, which would start with lab tests and eventually include hospitalizations and other medical information.
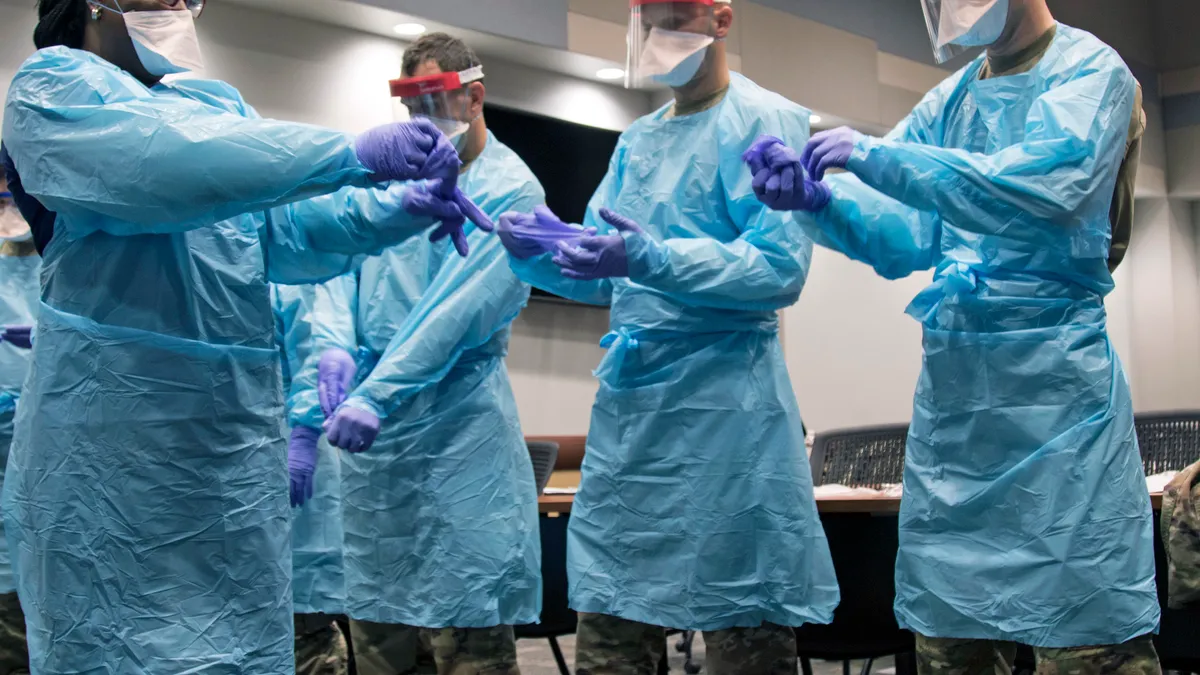
However, the tranche of funds would not flow to private labs, which say they are struggling financially facing rising costs for supplies like swabs, reagents and personal protective equipment, and flagging revenue as non-COVID-19 testing grinds to a halt.
ACLA asked for $5 billion in emergency funding for U.S. labs to bolster their testing efforts in March. But administrative and congressional action to date has not benchmarked any funds specifically for commercial labs to support COVID-19 testing. But both private and public labs are struggling with the deficit.
"Many times our public health labs only have the opportunity to update their systems when they receive grant funding or there is a national or international infectious disease threat," said Patina Zarcone, director of informatics at the Association of Public Health Laboratories, noting labs need a more consistent stream of funding to remain up-to-date.
CMS on Wednesday did roughly double the Medicare reimbursement rate for high-throughput COVID-19 molecular tests from $51 to $100 to expand testing availability nationwide, as roughly 650,000 Americans have tested positive for the virus. But that money will only go so far, experts say, without a coast-to-coast, interoperable reporting system to ease some of the burden currently resting on the shoulders of providers, commercial labs and public health agencies from the local to federal level.
"A national emergency warrants a national response," Sequoia Project CIO Debbie Condrey said.