Dive Brief:
- CMS is proposing to deploy an additional Medicare payment to providers for at-home dialysis treatment, particularly for new and innovative dialysis machines used in the home.
- The agency said Monday the need for more at-home care as never been more urgent, especially for those with underlying health conditions like end-stage renal disease. In fact, CMS said the ESRD population has the highest rate of hospitalization due to COVID-19 among Medicare beneficiaries.
- The proposed rule outlined two applications CMS received for the Transitional Add-on Payment Adjustment for New and Innovative Equipment and Supplies (TPNIES) from industry incumbent Baxter and startup Outset Medical. The latter announced $125 million in Series E funding in February, but neither have yet gained the agency's full support.
Dive Insight:
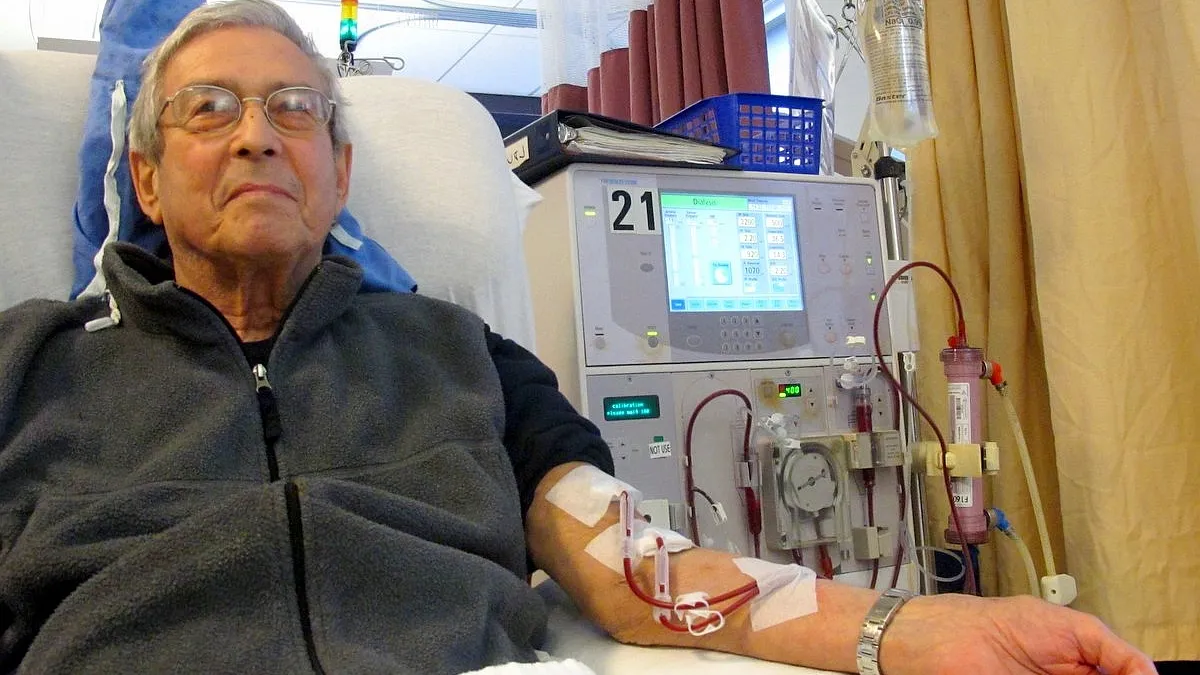
A substantial portion (85%) of fee-for-service Medicare members with ESRD go to an outpatient facility about three times a week, on average about 12 hours each week, to use a machine that filters the toxins from their blood.
Aspects of the proposed rule this week builds on efforts by the Trump administration to shift how the U.S. pays for and treats patients with kidney disease.
Last year, the administration launched a three-pronged plan dubbed Advancing American Kidney Health to reduce the number of Americans with ESRD by upping preventative care, establishing incentives for at-home care and increasing organ transplants. Around that time, companies including Baxter and CVS announced growing efforts in at-home dialysis technology.
CMS also launched a handful of new payment models, most of them voluntary, to achieve these goals.
Two companies applied this round for the Transitional Add-on Payment Adjustment for New and Innovative Equipment and Supplies. The agency found Baxter's Theranova 400 and 500 dialyzers did not yet demonstrate sufficient evidence of substantial clinical improvement (SCI) for Medicare dialysis patients, but welcomed further evidence in the comment period.
"Despite this setback, the potential for differentiated reimbursement for Theranova still exists," analysts at UBS said in a note this week, adding Baxter has invested $25 million in developing clinical evidence and will submit comments to the agency by the end of August.
As for Outset Medical's cartridge for use with its Tablo hemodialysis system, CMS concluded that while the technology is "a promising concept to encourage home HD," it may not meet the agency's criteria for SCI.
"There does not appear to be a need for this cartridge in the hospital or clinic setting as trained personnel should be able to assist with set-up," the proposed rule says. "Within the larger policy context of FDA approval and the fact that TPNIES does not currently cover capital-related assets, the CMS TPNIES Work Group believes there are some irregularities and misalignments in the current application." The agency is seeking public comment on whether Outset's technology simply meets the SCI criteria for the payment system.
A large chunk of the U.S. has some form of chronic kidney disease, and many of those patients have multiple underlying chronic conditions, complicating their health status. About 15% of adults in the U.S., or 37 million people, have chronic kidney disease, according to estimates from the Centers for Disease Control and Prevention.
Next year, the Trump administration expects to spend $10.3 billion paying 7,400 treatment centers for dialysis treatment. CMS also is proposing to bump up the base payment rate by about $16 to nearly $256.
"In the midst of a deadly pandemic that poses a particular threat to those with serious underlying conditions, President Trump's call for increased access to home dialysis has never been more urgent," CMS Administrator Seema Verma said in a statement. "Unfortunately, government rules too often stand in the way. Today's action represents a sorely needed course direction, making it easier for ESRD facilities to make new and innovative home dialysis machines available to patients who need them."