Dive Brief:
- Mental health advocates and insurers watched closely this week as CMS revisited and moved a step closer to paying for vagus nerve stimulation for treatment-resistant depression, a device therapy approved by the FDA in 2005.
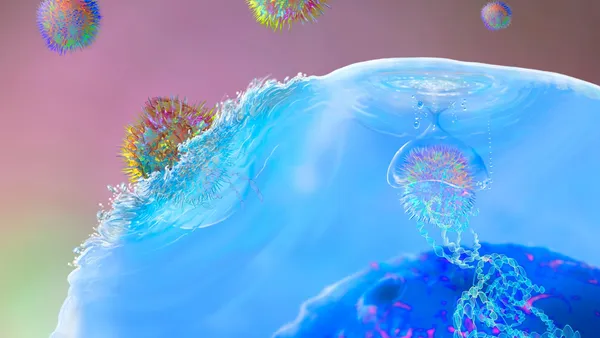
- The treatment, sold by U.K. medtech manufacturer LivaNova, is a surgically-implanted, pacemaker-like device that sends mild electrical pulses to the brain via the vagus nerve, one of 12 pairs of cranial nerves. Proponents of the device view it as a viable alternative for adults experiencing a major depressive episode who have not responded adequately to four or more antidepressant treatments.
- CMS announced in a Proposed Decision Memo late Monday that it would move forward with the device through its Coverage with Evidence Development pathway, requiring a randomized clinical trial before making a final decision on broader coverage.
Dive Insight:
CMS has moved LivaNova closer to widespread coverage, but not given the company immediate gratification. LivaNova stock was down 18% Tuesday following the update to the coverage decision.
The agency last considered covering the treatment for serious depression in 2007, when it concluded that evidence for the product's effectiveness was not compelling enough to expand coverage. Vagus nerve stimulation (VNS) is currently only covered by CMS for drug-resistant epilepsy.
The FDA-approved product was manufactured by Cyberonics, which is now a subsidiary of London-based LivaNova.
Ten years and some research later, CMS said that existing evidence shows enough potential to warrant a CMS-approved randomized clinical trial lasting a minimum of one year.
A five-year study of VNS for treatment-resistant depression (TRD) released in 2017 showed that patients with chronic moderate to severe TRD experienced anti-depressant effects at a significant rate when treated with the therapy.
"Based on the evidence, we believe that VNS for TRD seems promising but not convincing," the CMS memo issued this week said. "To ensure benefits to Medicare beneficiaries we are proposing to cover VNS for the treatment of TRD when offered in double-blind, randomized, placebo-controlled studies."
LivaNova says that's still good news, calling it "a positive step toward increased access to important therapies for these patients," in a press release Tuesday.
If clinical trial outcomes prove positive, VNS-related costs could be covered under CMS' physician services, hospital services and durable medical equipment categories.
That would open a big market for LivaNova, gaining access to the 11% of Medicare beneficiaries that CMS said have had some depression diagnosis filed on their behalf. Of those 6 million people, an estimated 10% to 33% will likely exhibit characteristics of TRD.
Jefferies analysts estimated this Medicare population opportunity alone to be worth approximately $30 billion, based on a cost of $25,000 per VNS implant, in a note to investors.
Private insurers often look to CMS for coverage guidance. But at least one major insurer is not enthused about the evidence.
Anthem called the medical literature "incomplete" and inadequate in addressing associated risk, and asked CMS to refrain from an immediate decision to cover VNS more broadly for TRD patients, in a public comment.
The insurer was among the 36 individuals and organizations who submitted feedback during the initial comment period from May 30 to June 29 this year.
Conversely, mental health advocacy groups welcomed the shift toward coverage. Nathaniel Counts, senior policy director at Mental Health America, commented in support of the revisited NCD, and said his organization is pleased by this week's update.
"It’s exciting to see CMS evaluating evidence for the broader range of therapies to treat mental health conditions," Counts said, adding that the move indicated “positive steps” toward incorporating further evidence into interventions.
The comment period for the proposed decision will remain open until Dec. 19. LivaNova says it will begin the clinical trial once CMS finalizes the NCD, which is expected on or before Feb. 17, 2019.