Dive Brief:
-
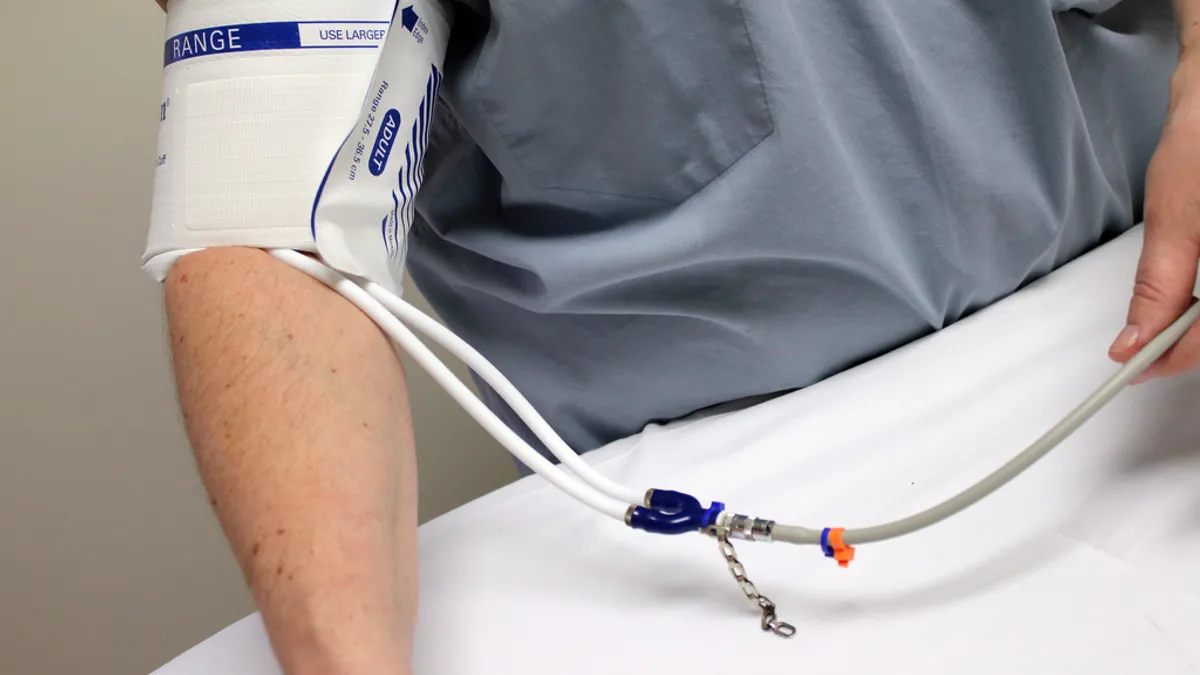
CMS has finalized changes to the coverage of ambulatory blood pressure monitoring (ABPM) to permit testing of patients with suspected masked hypertension.
-
Under the new rules, CMS will reimburse physicians for ABPM performed when they suspect blood pressure readings taken from a patient in a clinical setting are artificially low.
- The final decision covers the same key points as the draft released in April but features some changes, such as the removal of a requirement that patients undergo three months of behavioral interventions before ABPM.
Dive Insight:
Under its old policy, CMS covered ABPM in patients with suspected white coat hypertension. Blood pressure readings taken from such patients in clinical settings are higher than their real-world figures, creating the risk that they will be treated unnecessarily for hypertension unless ABPM is performed. However, CMS did not cover ABPM in patients with the opposite syndrome, masked hypertension.
Following recommendations from the U.S. Preventive Services Task Force and a formal request from medical associations, CMS has now changed its policy to cover masked hypertension.
The final decision diverges in several areas from the draft proposal CMS released for consultation. In finalizing the policy, CMS has removed the requirement for patients with suspected white coat or masked hypertension to undergo behavioral interventions, such as diet and exercise modification, before receiving ABPM.
Other revisions made by CMS also affect its policies on both white coat and masked hypertension. Notably, CMS dropped a requirement for ABPM devices to be certified and validated for use in the intended patient population by the dabl Educational Trust or a similar blood pressure monitoring quality control organization. CMS retained other requirements on the choice of ABPM devices.
CMS also tweaked its definition of suspected masked hypertension. The final decision states patients are suspected to have the condition when they present with average office systolic blood pressure between 120 mm Hg and 129 mm Hg or diastolic blood pressure between 75 mm Hg and 79 mm Hg, plus at least two measurements of greater than 130/80 mm Hg taken outside a clinical setting.
The definition underwent minor changes in the finalization of the policy. The bigger change over the old text was put forward in the draft and retained in the final policy. Whereas CMS previously used 140/90 mm Hg as the threshold for hypertension, it has now adopted the lower definition of 130/80 mm Hg.
Coupled to the coverage of ABPM for suspected masked hypertension, the threshold change could result in more patients being treated for hypertension. The medical groups that asked CMS to look at its ABPM policy argued changes to diagnostic practices were need in light of the cost of cardiovascular disease.