As a plethora of wearable devices hit the market, able to track everything from a patient’s cardiac rhythms or walking gait to blood glucose levels, why can’t implants do the same? That’s the crux of the idea behind Canary Medical, which implanted its first sensor in a patient last year. The company developed an embedded sensor that works with Zimmer Biomet’s knee implants. The sensor, about the size of an AA battery, can track a person’s steps, walking speed, stride and range of motion.
Bill Hunter, a physician in Vancouver, founded Canary in 2012 with the idea that if smartphones could track health metrics, such as people’s steps and heart rate, technology could be brought into implants, to track a patient’s progression after a surgery or to warn if an implant is failing.
Earlier in his career, while he was finishing medical school, Hunter founded a company called Angiotech that combined drugs and medical devices, creating products like drug-coated stents. Now, with Canary, he is focused on incorporating sensors into medical devices, starting with knees. He spoke in an interview about how the technology works and his long-term plans for the company.
This interview has been edited and condensed for clarity.

INDUSTRY DIVE: One of your first products is a knee implant manufactured with Zimmer Biomet. Why start with knees?
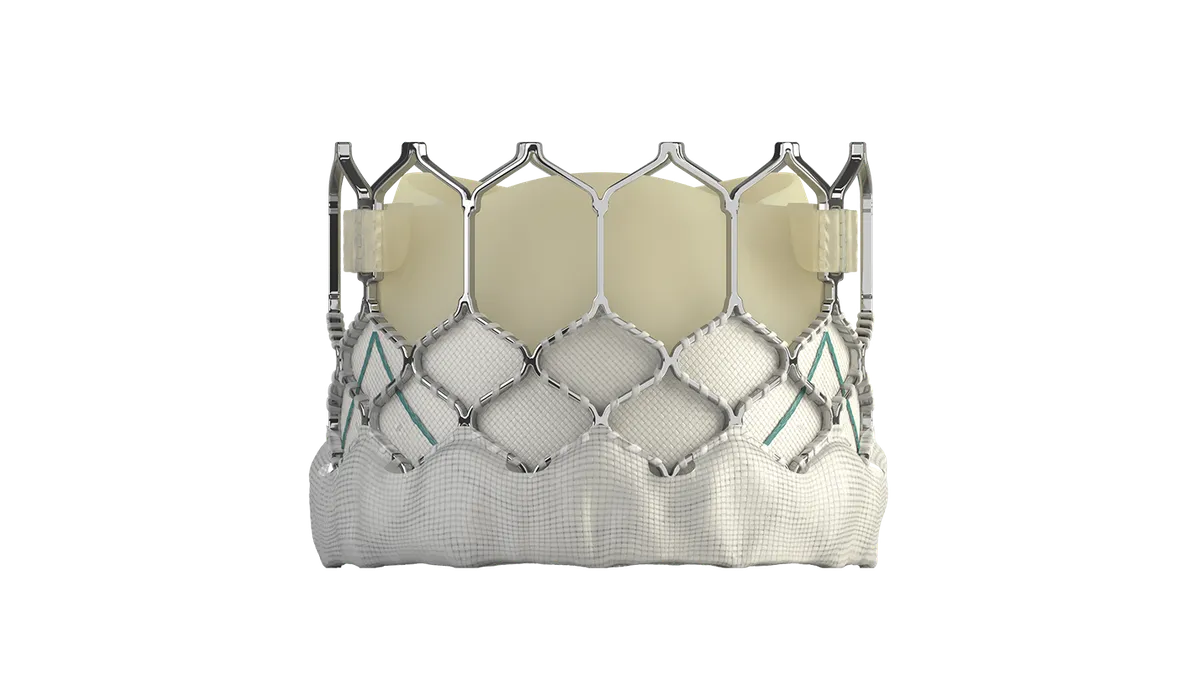
BILL HUNTER: When I was studying, my background was in coronary stents, so it was all in cardiovascular. And, in fact, the [implant] itself probably most closely resembles a pacemaker. Technologically, it was consistent with what we'd worked on for many years. [Now], the company is working on all kinds of different devices. But five or six years ago, the technology was still early in its evolution, we needed the space, and knees were big enough that we could get one of those little things in it. It wasn't that we woke up one day and said, ‘You know what? Orthopedics is going to be the killer app.’ It was that total knee joints are pretty big, and we had to use a pacemaker battery and telemetry, and all that stuff took up space. [In] a coronary stent, it wasn't technologically possible. In electronics, the speed of innovation and miniaturization is spectacular. So we will eventually get into other stuff, but initially the knee was what we were able to do.
How does it work?
It’s like a pacemaker battery: we're asking it to last for 10, 20 years, and we can't recharge it. If I transmitted [the data] in real time, so you were able to look at your smartwatch or your phone and see your stuff in real time, we'd be out of power within two or three days. [So] the power is only on from seven in the morning until 10 o'clock at night. Most of the time, the device is in low-resolution mode, collecting data at 25 observations per second. That's for doing step count, cadence, stride length, macroscopic activity, if you will. And then three times a day it goes to 800 observations per second. That’s when we do gait, range of motion, very precise measurements, but we only do those three times a day and we only do them for short periods of time because that takes power. And then last but not least, you have to transmit that data, which also takes power. We only do that once a day. So if you want to see your data, you're only going to see what you did yesterday.
Over the first year, we collect data every single day, but we back off in the future. We collect it only a few months a year over the next few years because at that point, your doctor is just looking to see if there are any changes from baseline. We do all these things to conserve power. The biggest part of this is the battery, so the less power you need, the smaller you can make the implant.
What are your ambitions for Canary? What other types of uses are you hoping to achieve with this technology?
The way I look at it is that from the first day of the first patient, you can become a monitoring company. On day one, we can start counting your steps and your cadence and your stride length and walking speed. As a clinician, we can tell the doctors, is my patient active or is my patient inactive? And, you know, recovering from a joint replacement, that's a fairly valuable piece of information. But that's all we can tell people at the beginning, because we don't have any frame of reference. As we get hundreds of patients, we start to understand the difference between normal and abnormal. We have a cohort of patients who recovered really, really well and we see what their typical data pattern and progression was like. Then we'll have some patients who fell behind or did poorly, and we'll see what their patterns were like. The goal is to be able to tell the clinician, not just is my patient active, but is my patient recovering the way I expect them to, or is my patient falling behind?
Once you have 10,000 patients, then hopefully you can tell them why they're falling behind. My patient’s falling behind because they have some soft tissue abnormalities, have a contraction, or maybe it looks like they're at high risk for developing an infection. The final step … if I have 50,000 patients, do I start to understand best practices? Do I start to understand what types of rehabs work, or what type of surgical techniques work in which types of patients? What’s the best method of caring for a person post-operatively?
Our hope is that as we gain this experience, and we have more and more datasets from more and more clinical conditions, then we can actually contribute to the discussion by giving the clinician diagnostic and potentially prognostic information. And each of those things is a separate submission to the FDA.
How long do you expect it will take to provide data-powered insights to physicians?
It really is the more common the event, the quicker you pick it up. In the development of the program, the rarer the event, the longer it takes and the more of those events that you're going to have to track. In the first year, we'll probably understand normal versus abnormal. In the second year, we'll start to understand why it's abnormal. Is this an infection? Is this a contracture? Is this loosening? Is this something like that? Because it's a bit of a numbers game.
What does the uptake look like from doctors and patients? I know it’s still pretty early days.
We're in the early adopter phase right now. We have a few clinicians who have put in a lot of them and so we've learned from those people. What we're doing right now, Zimmer refers to it as a limited release. The goal is to collect as good a dataset as possible, so right now, it's not about how many we're trying to sell to how many people, it's about trying to get the best results possible because ultimately those results will determine the quality of the product which will ultimately determine how attractive that product is to other doctors.
On the physician side, how do you manage it so it’s not just a bunch of data every day?
Giving the clinician more and more work is really not the object here. There's a graph of how the person is [performing] and are they above average or below average, so the doctors can see quickly how the patients are tracking. If you want to hover your cursor over and see exactly how many steps somebody took, the data is all there, but we don't bombard people with that kind of stuff.
We haven't submitted that part [to the FDA] yet. But what we would like to get to is a situation where you look at it quickly, you're like, okay, this person is all normal. Excellent. Or this person is falling behind in the following areas, is this somebody I need to take a look at? [We have] tried to make it very visual, something you can within two seconds look at and know what's going on.
Do you plan to use this same system for other implants?
We have patients right now with multiple implants. So, yes. It's actually been fascinating to see because we could see somebody recovering really well and all of a sudden, the person tailed off and we tried to figure out what was wrong and it turned out they had gone back to have their other knee done. All of a sudden we had two knees on the grid from the same patient.
Let’s talk reimbursement: What avenues are you looking at, both for the device and for the time physicians spend looking at the data?
CPT reimbursement codes already exist for using the data. So for monitoring your patients and using that data to come up with a treatment plan, the remote patient monitoring codes already exist. The device has been built to be compliant with those codes and allow the physicians to get paid for doing the remote patient monitoring. Using this as a diagnostic [tool] or using this to predict complications, those will all be separate CPT codes that will be based on data.
As for the device itself, even that's TBD. The knee falls within an entire procedure code under a [diagnosis related group] where you're paid for managing the patient from pre-op all the way to 90 days post-op. And so this potentially fits within that. However, as you can appreciate, the device works from day 91 to 20 years, which is well outside of that DRG. So I think even the device itself may end up with its own specific reimbursement.