Dive Brief:
- The American Kidney Fund lobbied the White House last week in a private meeting on a forthcoming HHS proposed rule on third parties providing financial assistance to end-stage renal disease patients. AKF, which gets the bulk of its funding from major dialysis providers DaVita and Fresenius, wants the government to allow patients to stay on private insurance.
- The insurance lobby and other groups such as the Service Employees International Union have worked for years to lobby HHS to reexamine policies they argue allow financially interested third parties such as the American Kidney Fund to steer ESRD patients eligible for Medicare or Medicaid into commercial coverage, especially COBRA coverage, allowing dialysis providers to profit from higher reimbursement.
- AKF President LaVarne Burton attended the White House meeting alongside its vice president of government affairs Holly Bode. The meeting was also attended by five HHS employees and five representatives from the White House Office of Management and Budget.
Dive Insight:
The meeting comes months after President Donald Trump issued an executive order seeking to overhaul U.S. kidney care by encouraging home dialysis and boosting kidney transplants with the goal of reducing the number of Americans with ESRD by 25% come 2030.
According to a publicly disclosed document, AKF argued at the White House meeting that ESRD patients waiting for kidney transplant should be able to stay on private insurance "because patients with private insurance are more likely to get a transplant." The group noted in 2018, approximately one in 20 kidney transplants were to patients receiving financial assistance from AKF.
AKF spokesperson Alice Andors told MedTech Dive the conversation with White House and HHS officials was not limited to how low-income dialysis patients receive kidney transplants. Since 2016, AKF has spent more than $2 million lobbying the federal government on a variety of issues, including charitable premium assistance
"We met with OMB staff to provide them with information about AKF and how our charitable premium assistance works," Andors said. "We also talked through the strict guardrails that we think any organization with a similar assistance program should follow to protect patients and the integrity of the program."
America's Health Insurance Plans told MedTech Dive in an email it is concerned that inaction by CMS and HHS to prevent patient steering will lead to increased costs for consumers in the individual market. AHIP took direct aim at private dialysis companies funding the AKF.
"An estimated 60% of DaVita Inc.'s pre-tax profit comes from patients with premiums funded by the American Kidney Fund, which is heavily subsidized by charity donations from DaVita (which qualifies as a charitable deduction)," the insurer trade group's spokesperson Cathryn Donaldson said in an email.
AHIP argues proposed regulations should mandate patient assistance funds be donated to a legally independent foundation without potential financial interests, disallow foundations from directing individuals to specific health plans and update conflict of interest standards to stop providers from referring patients to foundations that pay insurance premiums.
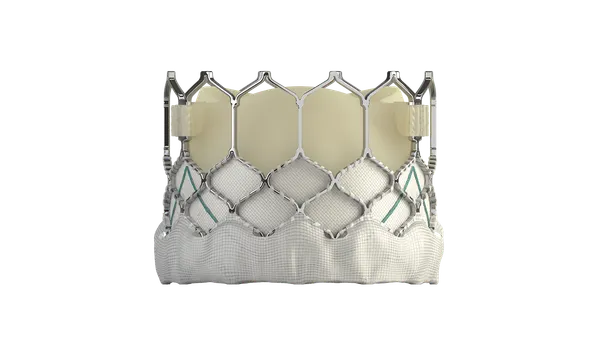
DaVita, one of the largest providers of dialysis care, currently provides home dialysis services to more than 26,000 patients, according to RBC. Another plank of the Trump administration's kidney reform efforts are five CMS payment models that aim to increase transplants, preventative care and at-home dialysis.
"On the regulatory front, [DaVita] appears well positioned for Trump administration efforts to increase home dialysis and transplant volume in theory, though management cites structural hurdles to the government's home penetration goals," an RBC equity research note said Friday. "While the company supports CMS' demonstration models in spirit, the details are critical."
Major medtechs such as Baxter have taken notice of the Trump administration's ESRD efforts. In July, Baxter announced it would pour $500 million of investment into at-home dialysis technologies and manufacturing facilities.
Comments on CMS' request for comments on its proposed mandatory payment treatment choices model for ESRD are due Sept. 16. Spokespeople from OMB and HHS declined to comment on the meeting.