The AMA Journal of Ethics has taken a deep dive into U.S. regulation of medical devices, raising questions about whether FDA is striking the right balance between supporting innovation and protecting patients.
In setting up the issue, Ariel Wampler, a plastic and reconstructive surgery physician at Lahey Hospital and Medical Center in Massachusetts, shared data on the regulation, use of and impact of medical devices. Most of the statistics date back years but still provide a snapshot of the case against the current approach. Wampler notes that less than 1% of medical devices went through two large clinical trials, as is standard for pharmaceuticals, from 2003 to 2007.
As it's typically easier and safer to discontinue use of a drug than an implant, Wampler suggests it "might be reasonable" to expect some devices be held to higher safety standards than pharmaceuticals.
Reported serious safety problems are exceedingly rare — less than 1% of devices cleared or approved between 2004 and 2009 have been subject to a Class I recall, though the recall system itself has also been criticized as being piecemeal and not comprehensive. Clinical trials of implants can be more complex, expensive and ethically problematic than studies of drugs.
Wampler and Anna Pisac and Natalia Wilson, the authors of an article in the journal issue, all picked up on criticism of the use of the 510(k) pathway. Pisac and Wilson quoted a study that found that between 1992 and 2012, 510(k)-cleared devices were 11.5 times more likely to face recalls than products with premarket approval.
"Furthermore, devices or materials have been cleared based on their substantial equivalence to predicates that were recalled due to adverse events, as was the case for 16% of surgical meshes cleared between 2013 and 2015," Pisac and Wilson wrote.
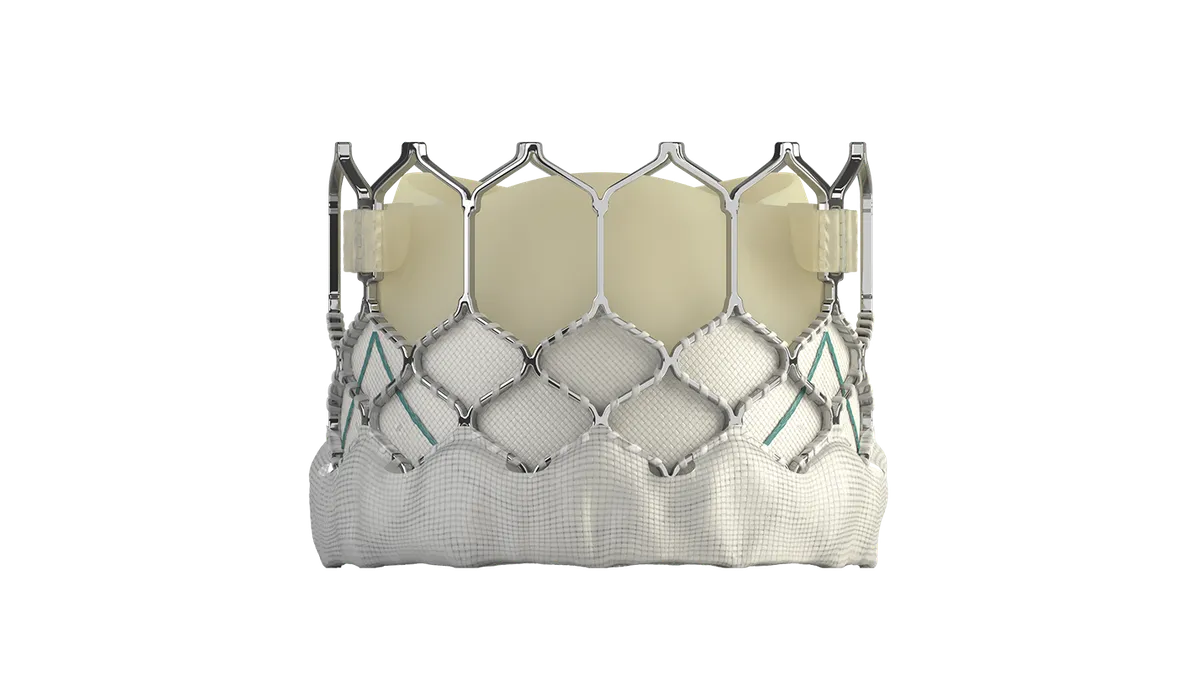
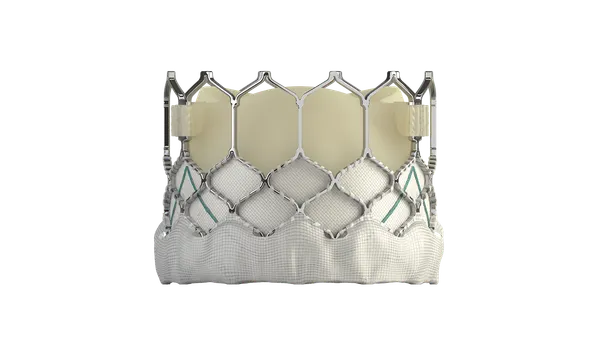
Surgical mesh products have a troubled history, leading to increased FDA oversight, an agency advisory panel and a call for more studies, amid tens of thousands of reports of serious adverse events and some deaths.
In 2019, FDA ordered Boston Scientific and Danish device maker Coloplast on Tuesday to immediately halt the sale of surgical mesh products indicated for transvaginal repair of pelvic organ prolapse after an agency advisory panel said there wasn't enough evidence that the products were safe.
The reliance on substantial equivalence, rather than evidence of safety and effectiveness, to support the clearance of devices via the 510(k) is a long-standing target of critics of U.S. medtech regulation. While the 510(k) pathway remains a key path to market, including for some implants, FDA has made changes in recent years, as Pisac and Wilson note in their article. Notably, FDA has restricted use of the pathway, introduced a "refuse-to-accept" policy and eliminated around 1,500 predicate devices.
Harvard Medical School’s Beatrice Brown and Aaron Kesselheim suggest a different approach on the question of how to manage questions about the safety and effectiveness of 510(k)-cleared devices. Brown and Kesselheim make the case that hospitals should hold off on bulk purchases of certain devices and get clinicians to discuss the benefits and risks with patients as part of a case-by-case approach.
"While hospitals might incur greater costs by not purchasing the devices in bulk, purchasing on a case-by-case basis can help avoid secondary costs — such as the use of hospital beds for additional procedures — if the device turns out to lead to worse outcomes for patients," Brown and Kesselheim wrote.
Women may disproportionately benefit from a new approach to devices. From breast implants to surgical mesh, many of the biggest device-related health concerns of recent years have affected women. In an article titled "Is the FDA Failing Women?," Madris Kinard and Rita Redberg identify areas of weak enforcement and compliance, such as a series of delays to the completion of breast implant postmarket surveillance studies.
Kinard, a former FDA staffer, and Redberg, a former member of an FDA expert panel, want to see better enforcement of postmarket surveillance, as well as the creation of a mechanism for reporting adverse events that is more accessible and user friendly to ensure transparency.