Dive Brief:
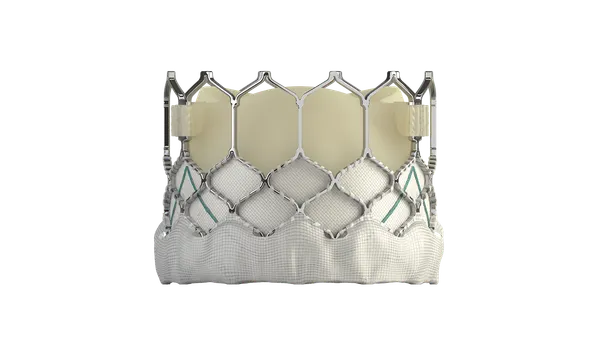
- AdvaMed in comments submitted to CMS is urging the agency to implement without further delay a regulation that would offer Medicare beneficiaries automatic four-year reimbursement coverage for medical technologies authorized under FDA's breakthrough device program.
- In response to CMS' decision to postpone the final rule from taking effect until May 15, AdvaMed argued that additional delays in implementing the policy could compromise access to breakthrough technologies for beneficiaries who face life-threatening or debilitating conditions without other treatment options.
- Rule skeptics, including patient safety groups and doctors, warn the rule goes too far and risks taking away the incentive to conduct clinical trials of the products.
Dive Insight:
The Medicare Coverage of Innovative Technology rule would provide national Medicare coverage of breakthrough devices for four years, starting at the time of FDA marketing authorization. At the end of the period, CMS would re-evaluate the technology based on clinical and real-world evidence of improved health outcomes and determine whether to grant permanent coverage.
But critics of the MCIT pathway contend the proposal could have the effect of promoting device use without rigorous evidence of safety and effectiveness, while also boosting healthcare costs. In a March perspective article published in the New England Journal of Medicine, doctors said the rule would undermine Medicare's authority to evaluate clinical evidence for device adoption.
CMS finalized the proposed regulation on Jan. 12 and planned to make it effective on March 15 before reversing course and postponing its implementation for 60 days to consider additional public input. When it announced the delay, the agency said it could revise, further postpone or even rescind the rule.
In a 13-page letter to CMS Acting Administrator Elizabeth Richter, AdvaMed argued the MCIT rule would "extend the spirit" of the 21st Century Cures Act by accelerating the coverage process and thus expediting access to breakthrough devices.
The industry group proposed CMS consider clarifying its definition of "reasonable and necessary" when determining Medicare coverage through a separate process in order to avoid holding up the MCIT rule. It also called for the use of existing coding and payment processes to avoid further delay in implementing the rule.
Benefit category determinations should not be an obstacle either, AdvaMed argued, because most Medicare claims are processed before there is national coverage. In addition, the group saw no reason to delay a decision to finalize the rule based on the potential volume of MCIT-eligible devices.
The American Clinical Laboratory Association, in comments to CMS submitted earlier in the rule-making process, voiced concern about the proposed definition of "reasonable and necessary," which includes "safe and effective" as the first criterion in the Medicare Program Integrity Manual, contending it should be struck from the regulation altogether to prevent an interpretation requiring laboratory developed tests (LDTs) to have FDA approval or clearance before Medicare can cover them.
ACLA, whose members include LabCorp and Quest Diagnostics, made the case that while the "safe and effective" standard is "appropriate for products distributed in interstate commerce that are designed for and intended to produce a direct therapeutic impact, LDTs are services, developed and performed by the same laboratory entity that do not create a direct therapeutic impact, but rather provide information to inform treatment decisions."