Dive Brief:
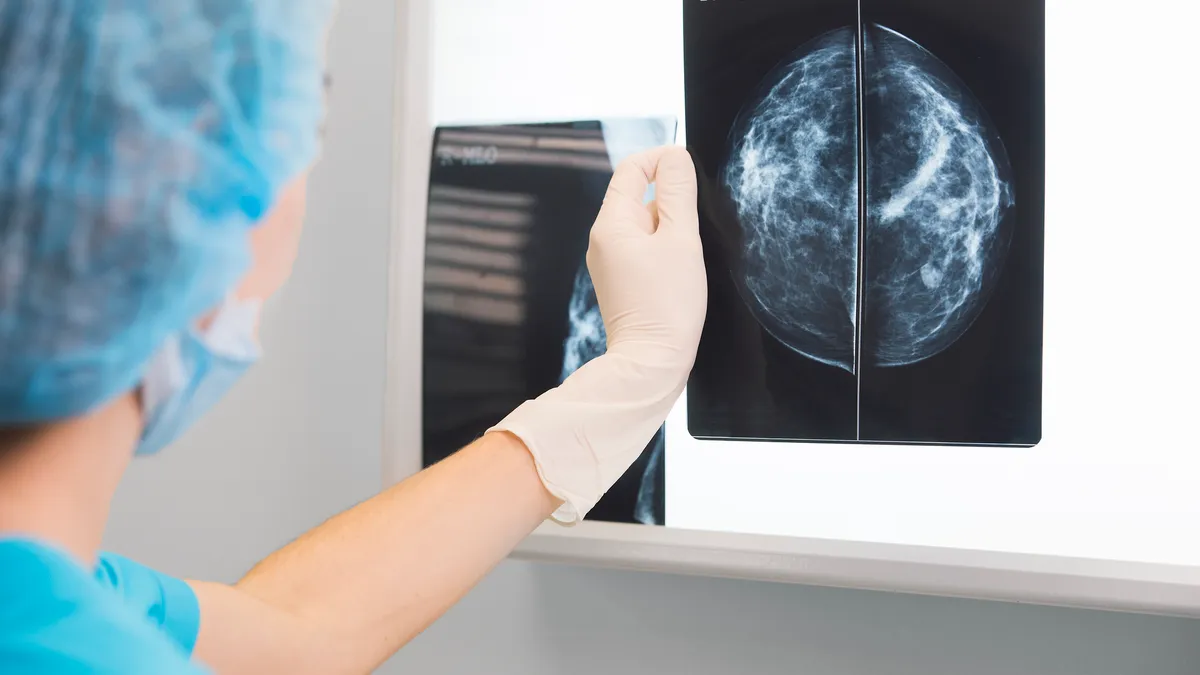
- Advamed has asked for Medicare to cover supplemental imaging of patients with heterogeneously and extremely dense breast tissue.
- In a letter sent to the Centers for Medicare & Medicaid Services Friday, the medtech industry group said many individuals with dense breasts currently have to pay out of pocket or forgo potentially life-saving additional testing.
- Advamed made the request two months after the Food and Drug Administration began requiring mammographers to notify patients when they have dense breast tissue. Traditional mammography is less sensitive than other imaging technologies in dense breasts, which increases the risks of imaging to miss cancer.
Dive Insight:
Nearly 50% of women aged 40 and older who get mammograms have dense breast tissue, according to the National Cancer Institute. Dense tissue can be harder to detect cancers on a mammogram, and it is also associated with an increased risk of cancer. Those factors led the FDA to update its mammography regulations to require facilities to notify patients about breast density.
Patients who learn they have dense breasts may undergo imaging with ultrasound, magnetic resonance imaging or contrast-enhanced mammography. However, Advamed said most Medicare beneficiaries lack coverage for supplemental imaging, with less than one-quarter of women in a plan that covers Medicare’s gap in services.
“Beneficiaries may either forgo supplemental imaging or are surprised by bills, especially when those exams were recommended and ordered by their healthcare provider,” Advamed CEO Scott Whitaker wrote in the letter. “In many cases, Medicare beneficiaries do not realize the costs associated with the imaging until it has already been performed.”
The trade group asked the CMS to ensure Medicare policies include density as an indication for coverage of supplemental breast imaging. Advamed also wants the CMS to reduce or eliminate cost sharing for patients whose providers have recommended supplemental breast imaging and to promote health equity via increased access to breast imaging modalities.
Around half of U.S. states have waived or capped cost sharing for women who must undergo additional imaging following a screening mammogram, according to the letter. Advamed said the CMS can “save lives in states without laws covering additional imaging” and set a precedent for state Medicaid programs and private health insurance plans.