Come early 2021, the medtech sector will have three quarters of data charting the downturn and recovery in the wake of COVID-19. Regardless of the path forward — a V, a W or something in between — the sharpest of impacts is expected to have peaked in spring 2020.
But the pandemic will no doubt shape medtech business decisions in the coming months and years as constraints on healthcare systems, economies and ways of working and living linger.
Below MedTech Dive lays out key areas of industry operations that the COVID-19 environment will likely affect in the year to come.
1. Direct-to-consumer campaigns
Ads hawking medical devices are far less common than for drugs, but a few companies have noticeably ramped up their direct-to-consumer efforts in recent years, including Boston Scientific with a rare medtech TV ad for an implant aimed at reducing stroke and Stryker making a social media play with elite athlete Alex Morgan.
While FDA has weighed in on ethics and best practices of direct-to-consumer advertising for drug manufacturers, it's less fleshed out for the device industry. AdvaMed has tried to get ahead of things, last year updating voluntary principles for marketers.
During COVID-19, the proliferation of DTC marketing by medtech companies has been multifaceted.
First, companies across the healthcare spectrum have launched broad campaigns urging consumers to return to seek care after distancing measures and fear over virus transmission in healthcare settings spurred a severe downturn in lucrative elective procedures.
LabCorp, Walgreens, Humana and others urged patients to Stop Medical Distancing this summer, for example. Hologic aligned with singer-songwriter Sheryl Crow with its Back to Screening campaign, encouraging consumers to schedule mammograms as healthcare facilities were reopening for imaging. Johnson & Johnson in September launched its own take on the effort dubbed My Health Can't Wait.
"We're really not focusing on any specific therapeutic area or any specific procedure," said Jijo James, chief medical officer at J&J Medical Devices, who worked on the campaign. It includes resources pointing patients toward telehealth options and suggestions on how to talk to a doctor about again seeking care.
Abbott took to the airwaves in April as it was being thrust into the national spotlight for its outsized role in America's coronavirus testing ramp-up. A 30-second TV spot looked to elevate the brand name while expressing gratitude to healthcare workers.
Separate from the COVID-19 theme itself, some companies saw the pandemic as an opportune time to target new customers, particularly as many spend more time engaging with media.
Dexcom, for example, is not slowing down its continuous glucose monitor marketing. "We'll continue to invest aggressively there to get the word out," said Matt Dolan, the company's head of new markets. "There's so many folks that that haven't even heard of it. And so it's very important that we continue to drive those campaigns."
Likewise, Exact Sciences CEO Kevin Conroy told investors in July the company expects to spend $70 million this year on television advertising alone. The company's signature product, colorectal cancer stool test Cologuard, remained an option for screening even as the rate of colonoscopies dropped dramatically.
That's one example of a medtech product that aligns well with the pandemic-driven expansion of telehealth. Jay Zhu, who leads the Medtech Commercial Strategy practice at Deloitte, said now is a time for those types of companies that typically compete with doctor's office or hospital-based treatments to capitalize.
"They see this as the golden opportunity for them to accelerate a shift" and are backing direct-to-consumer communication "to basically convince patients that now is the perfect time to use these kinds of less risky solutions."
A bit newer to consumer-focused advertising, Teleflex CEO Liam Kelly said this summer that as non-emergent procedures appeared to return, it decided to run a pilot national campaign from July to December for its UroLift device for enlarged prostate. "Our regional digital DTC efforts indicated strong patient engagement in June, along with positive sentiment from clinicians, both of which gave us confidence in the July launch," Kelly told investors.
2. Rethinking physical footprints
Like myriad other industries, distancing measures are reshaping where and how employees work, prompting medtech leaders to rethink their companies' footprints.
Stryker CEO Kevin Lobo told investors in July that while much of its capital spending in recent years went toward office buildings, particularly as Stryker has acquired companies and people, that trend is poised to change.
"We're going to embrace flexible work arrangements going forward, and we are not going to need the same real estate by any stretch that we have today," Lobo said. "Frankly, we're seeing a big change of what's going to be required in the future."
According to Eddie Rymer, a principal at commercial real estate firm Avison Young in medtech hub Minneapolis, many companies are taking a wait-and-see approach when it comes to making decisions. A "hybrid model" of embracing virtual work-from-home strategies part time for some employees while getting more essential workers back together is likely, Rymer said.
One strategy that Rymer is seeing implemented are sale leasebacks — when companies sell a building to investors to free up cash, only to lease it back instead.
JLL's Roger Humphrey, global lead of the firm's life sciences practice, echoed the current state of limbo. "A lot of our clients have put a lot of of their projects on hold, with respect to office space," Humphrey said.
And there's still the school of thought that medtech is competing with big tech for talent, and that attractive work environments remains a pull for winning top candidates. Humphrey, pitching a more optimistic outlook for real estate, noted that even as companies get more critical about how many people need to be working in the same space on a given day, the social distancing mindset and need to reduce density may balance that out.
On the manufacturing side, Humphrey thinks the supply chain lessons from the pandemic will continue to drive a desire for reshoring, and foresees Puerto Rico only growing in popularity. Humphrey also noted that North Carolina, Georgia and New Jersey are all potential targets for an uptick in medtech manufacturing, as they all have life sciences manufacturing infrastructure from 10 or 15 years ago before lots of production was transferred overseas
3. Remote medtech's post-pandemic future
Before the pandemic, remote programming and monitoring of an array of devices was becoming increasingly important. However, these features have become paramount.
Given unprecedented FDA regulatory flexibility, Medtronic, Philips, ResMed and others modified existing products so frontline providers could reduce virus exposure.
Medtronic worked with tech giant Intel and created a new remote management capability for its Puritan Bennett 980 ventilator to allow providers to adjust the breathing machine's settings outside of hospital intensive care units and away from patients.
"We're seeing hospitals talk about making that standard of care," Medtronic CEO Geoff Martha told investors during a late May conference call, adding that it's not a question of if that happens but when.
ResMed similarly developed cloud-based remote monitoring software for ventilators across Europe, providing clinicians with access to respiratory information using their smartphones.
FDA issued guidance in April expanding the remote monitoring and manual control of infusion pumps. In March, the agency also issued an enforcement policy, revised in June, to expand the availability and capability of non-invasive remote monitoring devices to support patient monitoring during the public health emergency. The guidance applies to legally marketed devices that measure and detect common physiological parameters, including electronic stethoscopes, oximeters, and EKG and blood pressure devices.
"The gist of the policy in this guidance is outlining how FDA does not intend to object to certain modifications to the indications, claims, functionality, hardware or software, of these devices" without prior submission of a premarket notification to the agency, said Jessica Paulsen, director of FDA's division of cardiac electrophysiology, diagnostics and monitoring devices.
Allowing manufacturers to change the indications or claims to allow for the use of devices in a home setting has been "a big one" during the pandemic, according to Paulsen.
Paulsen hastened to note that the COVID-19 guidance for non-invasive remote monitoring devices is one of many such policies issued by FDA only intended to remain for the duration of the public health emergency.
Still, some solutions will no doubt become permanent parts of the healthcare landscape after the crisis ends and FDA's emergency use authorizations have expired. Medtechs have either already sought out lasting FDA marketing authorization for such products or are in the planning process.
Philips in May received 510(k) clearance from FDA for a wearable biosensor to help monitor the heart and respiratory rate of hospitalized COVID-19 patients. The sensor, which has a CE mark, provides surveillance alerting clinicians of the risk of a patient's condition deteriorating.
Nearly overnight, COVID-19 has forever changed the status quo for how healthcare providers treat patients remotely with medtech. It's a trend that will continue to improve future care as the U.S. health system looks to drive down healthcare costs through remote monitoring and to increase patient access to care.
4. Clinical trials go remote
Remote technologies have also been extended to clinical trials — a trend that preceded the crisis but has accelerated since.
The scalability and deployability of the technology for clinical trials means that literally thousands of patients can be remotely monitored 24/7 to keep abreast of their conditions following a procedure involving the use of medical devices. All this patient-generated data is analyzed to establish clinically significant findings for devices in head-to-head or standalone studies.
"This is the wave of the future," said Brijeshwar Maini, national medical director of cardiology at Tenet Healthcare and professor of medicine at Florida Atlantic University.
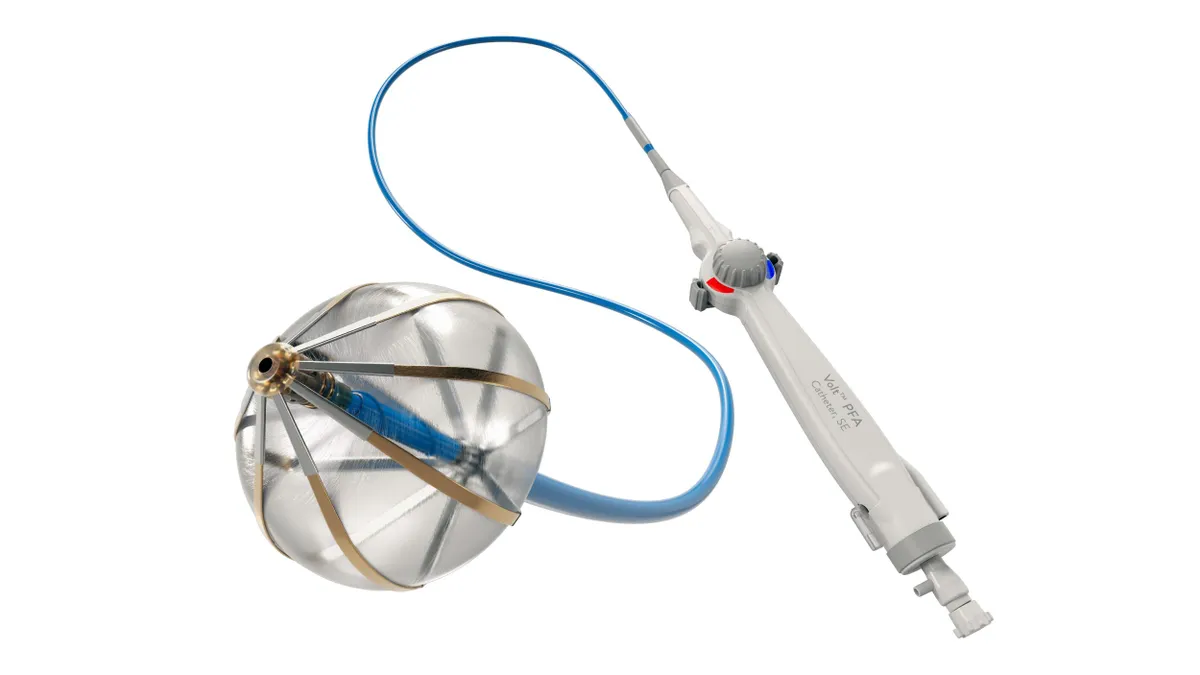
In particular, Maini sees the value of remote monitoring and telehealth to optimize clinical outcomes and increase patient satisfaction following transcatheter aortic valve replacement procedures.
Maini is principal investigator for a first-of-its-kind study of 100 patients undergoing TAVR whose primary objective is to measure the impact of these digital technologies on patient satisfaction, clinical outcomes and hospital readmission rates.
The prospective trial, Telemedicine for Symptom Tracking And Decrease Readmission Rate in TAVR Patients (TELESTAR-TAVR), will monitor patients in real time for cardiac arrhythmia — a predictor for readmission — and signs of early deterioration. Participating physicians will have discretion as to which TAVR devices will be used for specific patients.
Remote and wearable biosensor company VitalConnect is providing the technology including disposable patches used to monitor vital signs, EKG and 19 different arrhythmias, as well as a mobile device to transmit data from the patches to the cloud and a web-accessible central monitoring interface.
"All of those data points will be live streaming back to the caregiver's computer and central command station," said VitalConnect CEO Peter Van Haur.
Patients enrolled will be discharged within 24 hours of their procedure and monitored at home for seven days with the biosensor. They will then connect with their physician via video call and, finally, at 30 days, return to the hospital for follow up.
Maini points to a pivotal trial launched in 2019 to evaluate the safety and effectiveness of Abbott's TriClip transcatheter tricuspid valve repair system for the treatment of severe tricuspid regurgitation as an example of such remote patient monitoring. It is the first pivotal Investigational Device Exemption trial in the U.S. to evaluate a catheter-based, non-surgical treatment for patients with the condition.
In that Abbott trial, Maini notes that about 700 patients will be randomized to receive either the TriClip device or medical therapy and followed for a total of five years.
The TELESTAR-TAVR study, launched in September, was planned prior to the pandemic and ended up having a delayed start as a result of the outbreak, according to Maini.
COVID-19 has disrupted over 1,200 clinical trials and about a third have resumed, according to analytics company GlobalData. Although suspended trials have begun to recruit participants, GlobalData reports delays in trial initiation and slow recruitment continues.
"The clinical trials that could be conducted successfully on a remote basis were able to continue," observed Ira Bahr, COO of digital health company AliveCor. At the same time, Bahr said there are still some studies that are suspended "because they don't have the means of doing what needs to be done remotely."
Nonetheless, Kuldeep Singh Rajput, CEO of digital health company Biofourmis, which leverages a wearable medical-grade biosensor to gather patient data, said that despite the initial impact, about 80% of the clinical trials it is involved in have converted from traditional protocols to virtualized studies.
"Of course there were some hiccups earlier this year, but now those studies are going as planned and are recruiting patients," Rajput said.
FDA issued guidance in March, updated in September, for industry, investigators and institutional review boards on conducting clinical trials during the COVID-19 pandemic. Since trial participants may not be able to come to the investigational site for protocol-specified visits, the agency has recommended that sponsors evaluate alternative methods for safety assessments including virtual visits and remote monitoring.
"The market has fast-forwarded by almost five to six years" with the use of remote-virtual tech, commented Rajput. As a result, he says endpoints are being met much more quickly compared to the traditional ways of conducting clinical trials. "You can do continuous vital signs monitoring using sensors, so patients don't need to come back for office visits. And, you can do virtual visits now using telehealth capabiltiies," Rajput said.
5. HHS changes LDT policy for COVID-19 and beyond
For diagnostics, there may be no regulatory change over the course of the pandemic with potential for more disruption than the August decision that FDA will no longer require premarket review for laboratory-developed tests.
The HHS policy change said laboratories can voluntarily seek approval, clearance or emergency use authorization for an LDT, but they are no longer required to do so. The department cited regulatory flexibilities amid the pandemic as backing the change.
But experts like Scott Gottlieb, former FDA commissioner, warn the regulatory agency's ability to protect public health could be significantly impaired. Gottlieb on Twitter predicted a barrage of direct-to-consumer coronavirus tests will enter the market and be "processed in a central lab operating outside FDA oversight."
The change reverses a long-established FDA regulation and applies to all LDTs, not just COVID-19 diagnostics.
A senior AdvaMed official speaking on background called the move "the wrong call." The lobbying group is concerned that all diagnostic test developers, of both IVDs and LDTs, will not be subject to the same standard of testing validation during the pandemic and beyond.
While the American Clinical Laboratory Association, which represents companies most impacted by the LDT policy changes, said it appreciated HHS' recognition of flexibility for laboratories to innovate, the group argued it must be balanced with bringing to market quality testing services.
The Association for Clinical Oncology in September warned the HHS policy change threatens the safety of cancer care.
"The failure to develop reliable tests that perform as intended, could lead to patients receiving an inappropriate and potentially harmful treatment, or alternatively, not receiving a treatment that has the potential to be beneficial," said ASCO's Chair Monica Bertagnolli, who called for a regulatory framework that includes a risk-based approach to oversight in which LDTs are thoroughly validated.
Democratic lawmakers are looking into it as well. House Energy Committee Chairman Rep. Frank Pallone, D-N.J., in August demanded a briefing from HHS Secretary Alex Azar on the change.
Prior to the HHS policy change in August, Congress had been working on the regulation of LDTs. The Verifying Accurate, Leading-edge IVCT Development (VALID) Act introduced in March in both the House and Senate creates a new test product category, in vitro clinical tests, which include lab-developed tests, while giving FDA authority to review and approve IVCTs.
AdvaMed backs the legislation and is working with the bipartisan cosponsors in both chambers of Congress "so that all diagnostic tests are subject to the same modernized, risk-based, scientifically rigorous, and efficient regulations in order to ensure quality and patient safety."
Likewise, ACLA President Julie Khani in a statement said the VALID Act is critical to achieving "common sense, comprehensive diagnostic reform" through Congress that will enable "our ability to tackle the most challenging and complex health needs of the country."